Umbilical Cord Prolapse & Compression Injuries
What is umbilical cord prolapse?
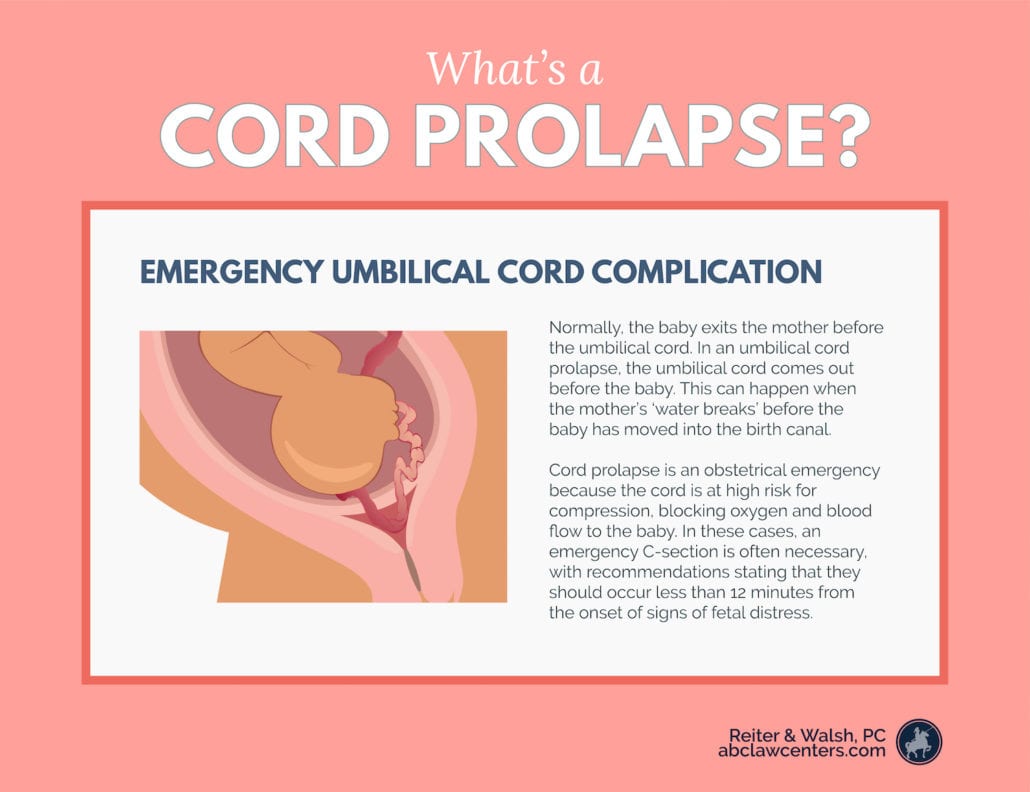
In an umbilical cord prolapse, the umbilical cord moves into the cervical canal, vagina, or comes out of the birth canal before the baby. When the baby comes down after the cord, the cord is compressed and the baby may not get enough oxygen. Umbilical cord prolapse is an obstetrical emergency because the cord is at high risk for compression. Cord compression can block oxygen and blood flow to the baby.
In cases of umbilical cord prolapse, an emergency C-section is often necessary. Cord prolapse occurs in about one in every 620 births.
Normally, the baby exits the mother before the umbilical cord.
Umbilical Cord Prolapse: Transcript
Another type of cord complication that can occur during labor and delivery is a cord prolapse in this situation, the baby’s head is not engaged in the pelvis. If the mom then has a rupture of membranes, it leaves an opportunity for the umbilical cord to fall through and deliver before the head. This is an emergency situation.
Once this happens, any part of that baby—whether it be the head, the shoulder, or the body—will start to occlude the umbilical cord and cut off the oxygen source to the baby. The baby quickly develops hypoxia and eventually will develop hypoxic-ischemic encephalopathy (HIE).
Types of umbilical cord prolapse
There are two types of umbilical cord prolapse:
- Overt prolapse: This is the most common type of cord prolapse. It happens when the cord comes out of the cervix or vagina before the presenting part of the baby. The cord is either visible or able to be felt by the medical practitioner.
- Occult prolapse: This happens when the cord descends alongside, but not past, the presenting part of the baby. It can happen with ruptured or intact membranes.
What causes a cord prolapse?
There are several causes of umbilical cord prolapse. These include:
- Premature rupture of the membranes (PROM): This is the most common cause. If membranes rupture early, or a physician artificially ruptures the membranes (an amniotomy), the baby’s head may be high up in the uterus. The umbilical cord can emerge through the cervix before or alongside the baby. The cord can then become compressed as the baby descends.
In cases where PROM occurs before 32 weeks, cord compression occurs 32-76% of the time (2). - Prematurity: Premature infants have a higher risk of malpresentation. The babies also tend to be smaller. Premature pregnancies may have a high volume of amniotic fluid in relation to the baby’s size).
- Multiples (twins, triplets, etc.): The first baby may push out the cord of another baby upon exiting the mother.
- Abnormally long cord
- Low birth weight
- Low lying placentation
- Pelvic deformities
- Prolonged labor
- Unengaged presenting part
- Uterine malformations
- External fetal anomalies
- Polyhydramnios (excessive amniotic fluid): When there is a large volume of fluid, the cord can be forced out before the baby. The pressure of the fluid exiting the mother can cause cord prolapse.
- Malpresentation
Tell us your story.
A birth injury diagnosis is difficult on your family. Call the birth injury attorneys at ABC Law Centers: Birth Injury Lawyers. We will listen to your story, answer your questions, and help build a sustainable future for your child.
Signs and symptoms of cord prolapse
The most obvious symptom of a prolapsed umbilical cord is seeing or feeling the cord before the baby is delivered. Fetal distress from lack of oxygen can also be observed as a sudden and prolonged fetal heart rate deceleration on the fetal monitor (bradycardia). This can also be a sign of other equally serious delivery problems and requires immediate attention from medical staff.
An ultrasound or fetal Doppler can diagnose umbilical cord prolapse and compression before labor. During labor, a medical professional can diagnose these issues by touching the umbilical cord and recognizing abnormalities in the fetal heart rate.
Treatment for umbilical cord prolapse
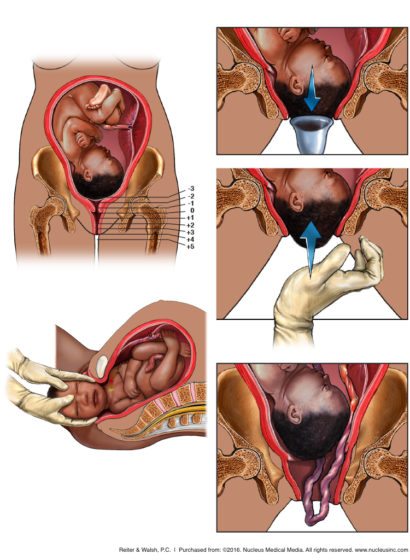
Once a prolapse is diagnosed, it requires rapid emergency delivery. In some cases, a physician will try to move the baby away from the cord. The movement can sometimes relieve the pressure and reduce the risk of oxygen deprivation during a vaginal delivery attempt. Sometimes, medical staff may try to expedite delivery with the help of forceps or a vacuum extractor.
Often this course of action doesn’t work. An emergency C-section should be performed immediately. To help prepare the mother for the surgery, the presenting part of the baby may be pushed back into the pelvis. These adjustments may continue to relieve the pressure from the cord.
If the delivery is not prompt, cord compression and prolapse can have severe effects on the fetus. When the cord becomes compressed, the fetus’s oxygen and blood supply diminishes or cuts off. This can lead to the bay not getting enough oxygen and hypoxic-ischemic encephalopathy (HIE), and brain injury.
Delivery must occur in minutes, usually by C-section.
Cord presentation before cord prolapse
A cord presentation (also known as a funic presentation) occurs when the umbilical cord presents before the baby. Doctors can identify cord presentation during routine prenatal care via fetal Doppler or ultrasound. Usually, a cord presentation before 32 weeks gestation is not a problem. If it persists after 32 weeks, medical professionals should examine the underlying cause and take precautionary measures.
Often, a funic presentation means that medical professionals will recommend a planned C-section. A scheduled procedure can prevent the baby from being injured.
Trusted legal help for umbilical cord prolapse, birth injury, and HIE

Has your child suffered brain damage from a lack of oxygen during delivery? Do you believe it was due to medical mismanagement of a prolapsed cord? If so, we encourage you to contact a law firm with experience in these types of complex cases.
ABC Law Centers: Birth Injury Lawyers was established to focus exclusively on birth injury cases. Since the firm’s inception in 1997, our legal team has addressed the needs of our clients in a variety of birth injury, pregnancy, and newborn medical malpractice cases. Our attorneys and in-house medical staff determine the causes of our clients’ injuries, the prognoses of birth-injured children, and areas of medical negligence.
Our attorneys handle cases all over the United States. Our birth injury team is also equipped to handle cases involving military medical malpractice and federally-funded clinics. Contact us today at (248)-593-5100.
Sources
- Bush, M., Eddleman, K., & Belogolovkin, V. (n.d.). Retrieved February 23, 2019, from https://www.uptodate.com/contents/umbilical-cord-prolapse
- Umbilical Cord Prolapse: Causes, Dangers and Treatment. (2015, November 30). Retrieved February 23, 2019, from http://americanpregnancy.org/pregnancy-complications/umbilical-cord-prolapse/
- WhattoExpect. (2018, November 15). Cord Prolapse During Pregnancy. Retrieved February 23, 2019, from https://www.whattoexpect.com/pregnancy/pregnancy-health/complications/cord-prolapse.aspx
- Siassakos, D., Hasafa, Z., Sibanda, T., Fox, R., Donald, F., Winter, C., & Draycott, T. (2009). Retrospective cohort study of diagnosis-delivery interval with umbilical cord prolapse: The effect of team training. BJOG: An International Journal of Obstetrics & Gynaecology,116(8), 1089-1096. doi:10.1111/j.1471-0528.2009.02179.x