Types of Umbilical Cord Problems
The umbilical cord connects a mother to her unborn baby; it is the baby’s only source of oxygen and nutrients, and also plays a critical role in removing fetal waste products.
Complications involving the umbilical cord may result in serious injuries in the infant, especially when medical professionals fail to provide proper fetal monitoring and care. Umbilical cord problems can cause birth asphyxia (dangerous oxygen deprivation), which can in turn lead to birth injuries such as hypoxic-ischemic encephalopathy (HIE) and cerebral palsy.
There are several distinct umbilical cord problems that medical professionals should identify and appropriately manage to avoid birth injury. These include:
- Umbilical cord compression
- Nuchal cord
- True knot
- Umbilical cord prolapse
- Short cord
- Vasa previa
- Intrauterine infections or chorioamnionitis
With all umbilical cord problems, early recognition (before an emergency situation occurs) is critical. Pregnancies with umbilical cord issues are considered high-risk and babies are often delivered early.
Types of umbilical cord complications
There are a variety of medical issues that can limit umbilical cord function. These include the following:
Umbilical cord compression
Umbilical cord compression occurs when pressure prevents the flow of oxygenated blood through the umbilical cord. Minor, periodic compressions are normal during uterine contractions. However, if the cord is compressed more than is typical, the baby can become brain damaged from oxygen deprivation, receive inadequate nutrition, or experience fetal acidosis (caused by an accumulation of carbon dioxide in the baby’s blood) (1). A variety of complications can lead to cord compression, including nuchal cords (2), true knot (3), and cord prolapse (1).
Nuchal cords
A nuchal cord is a complication that occurs when the umbilical cord wraps around the baby’s neck one or more times. This is common and occurs in about 15 to 35 percent of pregnancies. Often, nuchal cords do not impact pregnancy outcomes. However, certain types of nuchal cords can pose a significant risk to the baby. Nuchal cords can interrupt normal blood, nutrient, and oxygen exchange. This can lead to a variety of birth injuries, including hypoxic-ischemic encephalopathy (HIE), a form of brain damage caused by oxygen deprivation around the time of birth (4).
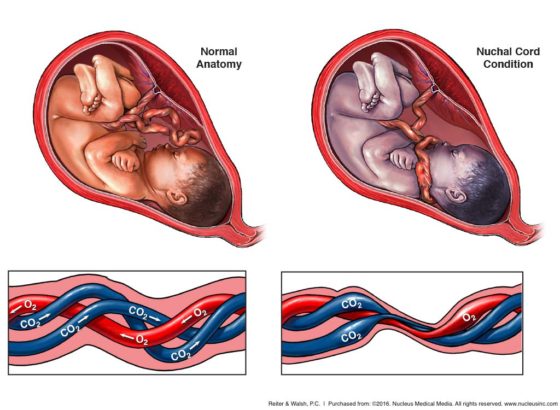
Nuchal cords interfere with oxygen flow through the umbilical cord
A nuchal cord is a complication that occurs when the umbilical cord wraps around the baby’s neck
True knots
When the umbilical cord forms a true knot, severe cord compression can occur, which can lead to serious birth injuries. Decreased fetal activity after 37 weeks of gestation is a common sign of a true knot (5). A nonreassuring heart rate will occur when the knot is serious enough to cause a lack of oxygen to the baby’s brain. True knots often occur in association with the following factors (5, 6):
- Pregnancy of monoamniotic twins
- Polyhydramnios (too much amniotic fluid)
- Having had two or more pregnancies in the past (multiparity)
- Long umbilical cords
- Small sized fetuses
- Male fetuses
- Gestational diabetes
- Amniocentesis
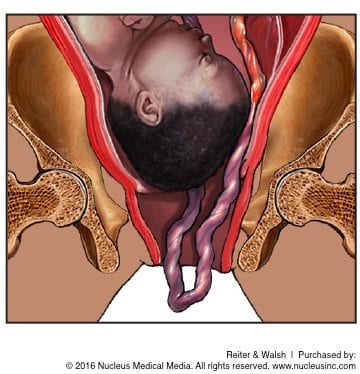
Umbilical cord prolapse
An umbilical cord prolapse occurs when the cord begins to slip through the birth canal ahead of (overt cord prolapse) or alongside (occult cord prolapse) the baby. Cord prolapse is a very dangerous complication because it can lead to cord compression (when the cord is pressed between the baby’s presenting part and the birth canal), birth asphyxia, and a variety of other serious birth injuries.
Medical professionals should be alert to the possibility of a cord prolapse, and prepared to intervene quickly if needed. They should be especially cautious when managing a pregnancy involving a cord presentation in the third trimester. Cord presentation describes a situation in which the umbilical cord is positioned between the baby and the birth canal. If this occurs prior to 32 weeks, it may resolve on its own, but if it occurs in the third trimester, intervention will likely be necessary (7). Doctors should carefully monitor the baby’s health and be prepared to perform an emergency C-section if the problem persists. With careful medical management, serious birth injuries and permanent disabilities can often be avoided.
Short umbilical cords
Short umbilical cords are at risk of stretching and rupturing. When there is a short cord, fetal movement may also cause excessive pulling on the placenta, causing it to tear away from the wall of the uterus (placental abruption). Placental abruption can cause severe maternal bleeding/hemorrhaging and can stop the baby from receiving adequate oxygen. In some cases, a short cord may also indicate a fetal health issue such as intrauterine growth restriction (IUGR). A short cord may be visible in a prenatal ultrasound. A baby with a short cord may also begin to show signs of fetal distress. Medical interventions for a short cord include both C-section and operative delivery (8).
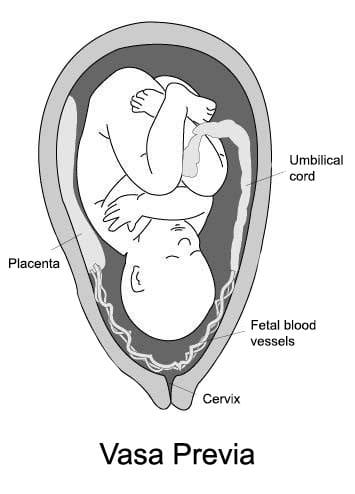
Vasa previa
Normally, fetal blood vessels in the umbilical cord connect the infant to the central region of the placenta. Vasa previa is a condition in which these vessels migrate out of the umbilical cord and into the amniotic sac membranes that lie across the opening of the birth canal.
Because of their position, these vessels are at risk of rupturing during labor and delivery. If the fetal blood vessels do rupture, it can lead to massive fetal blood loss and birth injury. Diagnosis is made by prenatal ultrasound. Mothers with a diagnosis of vasa previa should receive a recommendation for an early scheduled C-section delivery. When diagnosed during pregnancy, the rate of live birth is 97 percent. In the event that blood vessels rupture during delivery, the medical team should be prepared to provide a prompt blood transfusion to the baby (9).
Umbilical cord infection
Chorioamnionitis is an infection of the fetal membranes. Because chorioamnionitis can also spread to the umbilical cord, placenta, fetus, and amniotic fluid, it is now often also termed intra-amniotic infection or IAI (10). If IAI involves the umbilical cord, this is called funisitis. Funisitis can theoretically elicit fetal inflammatory response syndrome (FIRS). FIRS is said to be associated with a variety of serious fetal complications, including preterm birth, neonatal sepsis, periventricular leukomalacia (PVL), and cerebral palsy (11). Management with antibiotics and timely delivery are imperative when infection is diagnosed.
Prevention of umbilical cord problems
When umbilical cord function is impaired, the baby will likely exhibit signs of fetal distress (oxygen deprivation). These signs may be recognized through fetal heart rate monitoring (a “non-reassuring” heart tracing indicates distress) and a variety of other prenatal tests. If a baby is in distress, the medical team should intervene quickly. In many cases, an emergency C-section will be necessary. Physicians should always be prepared for this possibility.
Diagnosing umbilical cord problems before they cause birth injuries
Problems with a baby’s umbilical cord can often be diagnosed during prenatal testing. It is the standard of care to perform ultrasound exams of the umbilical cord during the second trimester or earlier if the mother has certain risk factors. In addition, if there is a long-term (chronic) umbilical cord problem that is causing oxygen and nutrient deprivation, prenatal tests may show decreased fetal movement and intrauterine growth restriction (IUGR). Dangerous umbilical cord problems and evidence of poor fetal well-being are almost always indications for early delivery. Any signs of fetal distress (oxygen deprivation) should also be taken very seriously.
Tell us your story.
Dealing with a birth injury diagnosis can be difficult, but our attorneys can help. Our team focuses exclusively on birth injury cases, and we can help you determine a future for your family. When you’re ready, give us a call.
Treating injuries caused by umbilical cord problems
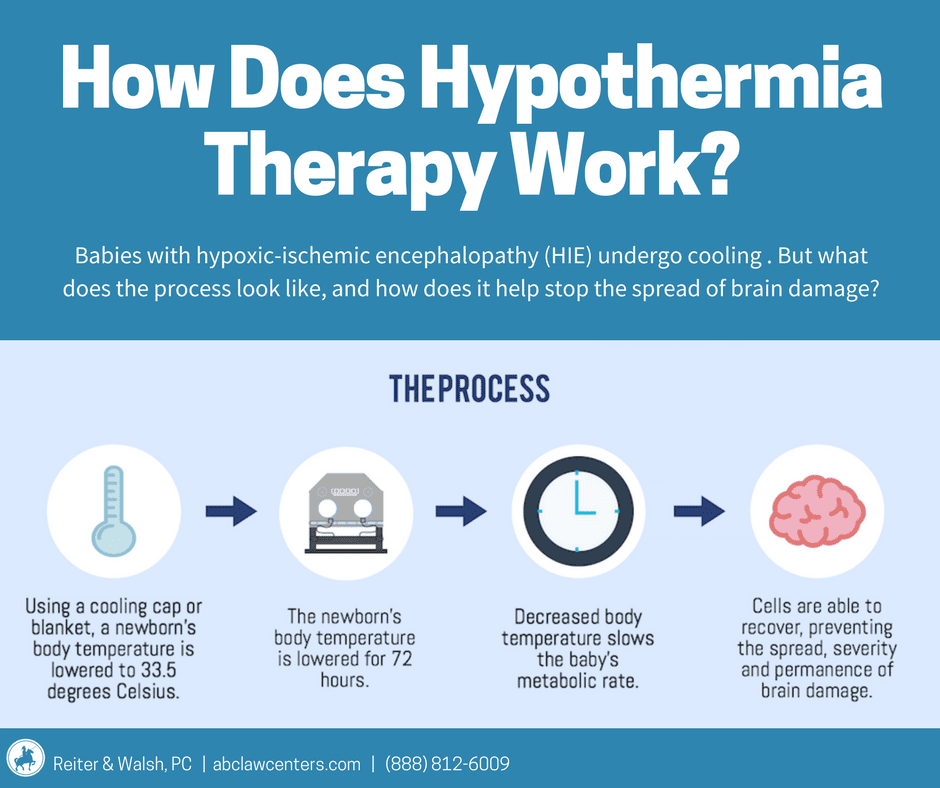
When umbilical cord complications cause hypoxic-ischemic encephalopathy (neonatal brain damage resulting from oxygen deprivation), doctors can treat the baby with therapeutic hypothermia (brain cooling).
During therapeutic hypothermia, the baby’s core body temperature is cooled to a few degrees below normal for 72 hours. Most guidelines dictate that this treatment must be given within six hours of the insult (usually birth asphyxia) that caused the HIE, which often means it must be given within six hours of birth. Research shows that therapeutic hypothermia halts almost every injurious process that starts to occur when the brain experiences a hypoxic-ischemic insult. It can prevent a baby with HIE from developing cerebral palsy, or it can reduce the severity of cerebral palsy.
Any other neonatal issues caused by cord complications (such as seizures or breathing problems) must also be promptly treated or the baby may develop further brain injury.
Trusted legal help for umbilical cord complications | our niche experience

If you’re seeking legal help for harm resulting from an umbilical cord complication, it’s critical to choose an attorney and firm that focus solely on birth injury cases. ABC Law Centers: Birth Injury Lawyers has been helping children with birth injuries since 1997. Our attorneys have won many awards for their advocacy of children and are leaders within the Birth Trauma Litigation Group (BTLG) and other industry associations.
We have helped children throughout the country obtain compensation for lifelong treatment, therapy, and a secure future, and we give personal attention to each child and family we represent. Our firm has numerous multi-million dollar verdicts and settlements that attest to our success, and clients pay nothing unless we win their case! Please reach out today to learn more.
Sources
- Umbilical Cord Prolapse: Causes, Dangers and Treatment. (2015, November 30). Retrieved July 31, 2018, from http://americanpregnancy.org/pregnancy-complications/umbilical-cord-prolapse/
- Nuchal Cord: What You Should Know. (n.d.). Retrieved July 31, 2018, from https://www.healthline.com/health/pregnancy/nuchal-cord
- Umbilical Cord Complications: Overview, Cord Length, Single Umbilical Artery. (2018, June 01). Retrieved July 31, 2018, from https://emedicine.medscape.com/article/262470-overview
- UpToDate, www.uptodate.com/contents/nuchal-cord.
- True Knot of Umbilical Cord. (n.d.). Retrieved February 2, 2019, from https://www.dovemed.com/diseases-conditions/true-knot-umbilical-cord/
- Ikechebelu, J., Eleje, G., & Ofojebe, C. (2014). True umbilical cord knot leading to fetal demise. Annals of medical and health sciences research, 4(Suppl 2), S155-8.
- Ahmed, W. A. S., & Hamdy, M. A. (2018). Optimal management of umbilical cord prolapse. International journal of women’s health, 10, 459.
- Short Umbilical Cord. (n.d.). Retrieved February 7, 2019, from https://www.dovemed.com/diseases-conditions/short-umbilical-cord/
- Everything You Need to Know About Vasa Previa (2017). Retrieved March 7, 2019, from https://www.healthline.com/health/pregnancy/vasa-previa
- UpToDate, https://www.uptodate.com/contents/intra-amniotic-infection-clinical-chorioamnionitis-or-triple-i
- Kim, C. J., Romero, R., Chaemsaithong, P., Chaiyasit, N., Yoon, B. H., & Kim, Y. M. (2015). Acute chorioamnionitis and funisitis: definition, pathologic features, and clinical significance. American journal of obstetrics and gynecology, 213(4), S29-S52.