Erb’s Palsy and Brachial Plexus Injuries
What is erb's palsy?
Erb’s palsy is a condition characterized by arm weakness or paralysis. It is often caused by pulling or pushing on the baby’s head during a shoulder dystocia delivery, which is a labor and delivery complication in which one of the baby’s shoulders gets stuck behind the mother’s pelvic bone. This may damage a network of nerves located near the neck, called the brachial plexus, and manifest in Erb’s palsy (1).
With proper medical management, brachial plexus injuries rarely occur. Therefore, the development of Erb’s palsy is often a sign of medical malpractice around the time of birth.
Risk factors for Erb’s palsy and brachial plexus injuries
Risk factors for Erb’s palsy and brachial plexus injuries include the following:
- Shoulder dystocia
- Fetal macrosomia
- Unusually short or prolonged second stage of labor (2)
- Maternal obesity
- Gestational diabetes
- Black race
- Induced labor
- Abnormal cervical dilation (3)
- A mother who previously delivered an infant with a brachial plexus injury
- Use of vacuum extractors or forceps (4)
- Cephalopelvic disproportion (CPD) (5)
- Usage of synthetic oxytocin (Pitocin) in labor
- Uterine tachysystole
- Fetal malpresentation (e.g. breech)
- Maternal age over 26.4 (6)
Causes of Erb’s palsy and brachial plexus injuries
difficult delivery and shoulder dystocia
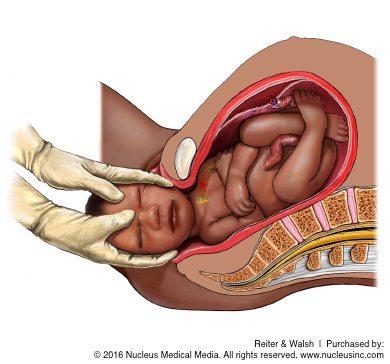
Several different forms of birth trauma can cause Erb’s palsy and brachial plexus injuries. The most common cause of Erb’s palsy is birth trauma associated with shoulder dystocia. Shoulder dystocia occurs when the baby’s shoulder gets hinged or stuck on the mother’s pelvic bone during delivery. It is diagnosed when the shoulders fail to deliver shortly after the head. When shoulder dystocia occurs, the doctor sometimes pulls too hard on the baby’s head, causing excessive strain on the baby’s shoulder and brachial plexus nerves. This strain can cause the nerves to tear or become severely damaged.
The dangers of forceps and vacuum extractors
Use of forceps and vacuum extractors to deliver babies increases the risk of shoulder dystocia. Doctors often lack the necessary skill and experience to utilize them properly. Frequently, when these devices are used, too much force is applied to the baby’s head. Forceps and vacuum extractors also put the baby at an increased risk of having an intracranial hemorrhage (brain bleed) and subgaleal bleeding (between the scalp and the skull).
Delivery during instances of dystocia
Use of excessive force or traction on a baby’s head during delivery is not necessary, and indeed, it is against the standard of care. If shoulder dystocia occurs, there are different types of gentle maneuvers physicians can perform in order to deliver the baby and prevent injury (click here for more information). Moreover, in many cases, delivery via C-section is safer. If risk factors for shoulder dystocia and brachial plexus injury are present, a C-section may be necessary.
Types of brachial plexus injury
Erb’s palsy affects the motion of the arm and shoulder more so than that of the hand and fingers, but any part of the upper limb may be involved.
When the lower brachial plexus nerves that control the hand and fingers are injured, it is referred to as total or global brachial plexus palsy. When primarily the hand and lower arm is affected, this is known as Klumpke’s palsy. Brachial plexus nerve injuries are often classified as such (7):
- Avulsion: Avulsion occurs when a nerve has been disconnected from the spinal cord. The connection will not recover.
- Rupture: Rupture occurs when the nerve has been stretched and torn (at least partially), but the damage is not at the spinal cord.
- Neurapraxia: Neurapraxia occurs when a nerve has been significantly compressed or stretched, but is still attached. There is a very good chance of rapid recovery.
- Axonotemesis: Axonotemesis occurs when axons are severed. There is a moderate chance of recovery.
- Neurotemesis: Neurotemesis occurs when an entire nerve is divided. There is a very slim chance of recovery.
- Neuroma: A neuroma is a tumor that grows from divided axons that haven’t regenerated. Prognosis varies.
Signs and symptoms of Erb’s palsy and brachial plexus injuries
The brachial plexus nerves carry signals from the brain to the arm, giving the arm instructions for how to move and perform certain tasks. If there is injury to the brachial plexus, the following signs and symptoms may appear:
- Abnormal arm movement
- Atrophy of muscles in the arm
- Limited sensation in the affected arm (e.g. the individual may be less responsive to temperature and pain in that arm)
- A broken clavicle (collar bone) or humerus (upper arm bone)
- Horner’s syndrome (in which the eyelid droops and the pupil of one eye is slightly smaller) (1)
- Pain in the affected arm (7)
- Absent Moro reflex on the affected side (8)
More specifically, Erb’s palsy is characterized by a ‘waiter’s tip hand’: the affected arm hangs limply from the shoulder, with the hand curled towards their rear.
Klumpke’s palsy is characterized by a “claw hand,” wherein the forearm is supinated (positioned so that the palm is facing outward) and the wrist and fingers are flexed. Klumpke’s palsy is sometimes associated with Horner syndrome (9).
Diagnosing Erb’s palsy and brachial plexus injury
A pediatrician is usually the one to make the diagnosis of Erb’s palsy, based on the weakness of the arm and physical examination.
The physician may order an x-ray or other imaging studies in order to assess whether there is any damage to the bones and joints of the neck and shoulder. The physician also may do some tests to learn whether any nerve signals are present in the muscle of the upper arm. These tests may include an electromyogram (EMG) or a nerve conduction study (NCS). To learn more about evaluation and diagnosis of brachial plexus injuries, click here.
Preventing Erb’s palsy through informed consent and birth planning
A main focus of brachial plexus advocacy groups is to encourage expecting mothers to ask their doctors about the risks of shoulder dystocia. A lack of informed consent is a major issue; often, doctors do not fully explain the risks of opting for vaginal delivery over cesarean section when shoulder dystocia is likely. The mother has a right to make an informed decision. This means that the doctor must explain the risks, benefits, and alternatives to every procedure that is considered.
Managing shoulder dystocia: The HELPERR Mnemonic
In vaginal deliveries involving shoulder dystocia, medical personnel must be very careful not to apply excessive force while trying to help the baby out because this can result in brachial plexus injuries and Erb’s palsy. Instead, physicians should follow the HELPERR mnemonic. These actions can be used in a variety of combinations, and do not have to be attempted in order; optimal management of shoulder dystocia depends on individual circumstances.
HELPERR stands for (10):
H – Help. A doctor can ask for help from other medical professionals.
E – Evaluate for an episiotomy. This is a procedure involving an incision in the mother’s perineum, between the anus and vagina.
L – Legs. A physician may ask the mother to pull her legs toward her stomach. This is known as the McRoberts maneuver.
P – Suprapubic pressure. A doctor may place pressure on a specific part of the mother’s pelvis to rotate the baby’s shoulders.
E – Enter maneuvers. This is another way of rotating the baby’s shoulders, but unlike suprapubic pressure, enter maneuvers involve internal rotation (the physician reaches the baby through the mother’s vaginal canal).
R – Remove the posterior arm. In this procedure, the doctor attempts to free one of the baby’s arms from the birth canal before the other.
R – Roll the patient. If the mother gets on her hands and knees, vaginal delivery may be more feasible.
Treatment for Erb’s palsy and brachial plexus injuries
Some babies recover on their own from brachial plexus injuries; however, more severe forms require treatment from specialists. Neonatal or pediatric neurosurgery is often required for certain types of injury Additionally, physical therapy is often required to regain muscle usage. Babies sometimes make a full recovery within 3-9 months. Patients who do not recover during this timeframe tend to have a lower likelihood of regaining function, because this may be indicative of avulsion (separation of the nerve from the spinal cord) (8).
The three most common treatments for Erb’s Palsy are:
- Nerve transplants: Nerve transplants (nerve graft surgery) are most often performed on babies under the age of 9 months since the rapid development of younger babies increases the effectiveness of the procedure. It is not generally done on older infants since it is riskier and may result in nerve damage in the area from which the nerves were taken.
- Subscapularis releases: These procedures involve cutting a “Z” shape into the subscapularis muscle to provide stretch within the arm. It can be done at any age and may be performed repeatedly on the same arm. This procedure, however, compromises the integrity of the muscle.
- Latissimus Dorsi Tendon Transfers: This involves cutting the Latissimus Dorsi in half horizontally. Then, part of the muscle is pulled around and attached to the biceps. This procedure provides external rotation, but may sometimes cause increased sensitivity of the part of the biceps where the muscle will now lie (11).
Long-term effects of Erb’s palsy and brachial plexus injuries
While many Erb’s palsy injuries heal on their own, a baby with Erb’s palsy will require frequent re-examination to confirm that the nerves are recovering. Depending on the injury, recovery can last for an extended period of time. Early in a baby’s life, parents may need to perform rehabilitative exercises, which can limit permanent harm.
In minor cases, full range of motion is often restored. However, children with more severe brachial plexus injuries usually never have a full range of motion.
In the long-term, some children may experience abnormal arm muscle growth as a result of Erb’s palsy. The restriction in growth generally results from comparative lack of use of these body parts and the influence of nerves (unaffected vs. affected) on growth. The lack of muscular development in areas affected by the brachial plexus may lead to long-term weakness or lack of movement. Similarly, these areas may experience abnormal circulatory development resulting in an inadequate ability to regulate temperature in these areas as compared to the rest of the body. Lack of circulatory development can also reduce the healing ability of the skin. Skin may take greater periods of time to heal and infections may easily manifest if open cuts or injuries are not sterilized immediately. Arthritis is another potential long-term effect of Erb’s palsy.
The above information is intended to be an educational resource. It is not meant to be, and should not be interpreted as medical advice.


Trusted birth injury lawyers
If your child was diagnosed with a birth injury, such as Erb’s palsy, cerebral palsy, a seizure disorder, or hypoxic-ischemic encephalopathy (HIE), the award-winning attorneys at ABC Law Centers: Birth Injury Lawyers can help.
We have helped children throughout the country obtain compensation for lifelong treatment, therapy, and a secure future, and we give personal attention to each child and family we represent. Please reach out today for a free case evaluation.
Featured Videos
Posterior Position
Hypoxic-Ischemic Encephalopathy (HIE)

Featured Testimonial
What Our
Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on. ABC Law Centers: Birth Injury Lawyers was just that.
- Michael
Helpful resources
- (n.d.). Retrieved October 9, 2018, from https://www.rch.org.au/kidsinfo/fact_sheets/Brachial_plexus_palsy/
- Chater, M., Camfield, P., & Camfield, C. (2004). Erb’s palsy–Who is to blame and what will happen?. Paediatrics & child health, 9(8), 556-560.
- Weizsaecker, K., Deaver, J. E., & Cohen, W. R. (2007). Labour characteristics and neonatal Erb’s palsy. BJOG: An International Journal of Obstetrics & Gynaecology, 114(8), 1003-1009.
- Erb’s Palsy. (n.d.). Retrieved October 9, 2018, from http://www.aanem.org/Patients/Disorders/Erb-s-Palsy
- Bhat, V., & Oumachigui, A. (1995). Nerve injuries due to obstetric trauma. The Indian Journal of Pediatrics, 62(2), 207-212.
- Louden, E., Marcotte, M., Mehlman, C., Lippert, W., Huang, B., & Paulson, A. (2018). Risk Factors for Brachial Plexus Birth Injury. Children, 5(4), 46.
- Kieffer, S. (2017, September 27). Brachial Plexus Injury (BPI) | Nerve Injuries and Symptoms | Johns Hopkins Peripheral Nerve Surgery Center. Retrieved October 9, 2018, from https://www.hopkinsmedicine.org/neurology_neurosurgery/centers_clinics/peripheral_nerve_surgery/conditions/brachial_plexus_injury_bpi.html
- Brachial plexus injury in newborns: MedlinePlus Medical Encyclopedia. (n.d.). Retrieved October 9, 2018, from https://medlineplus.gov/ency/article/001395.htm
- (n.d.). Retrieved October 9, 2018, from https://www.uptodate.com/contents/neonatal-brachial-plexus-palsy?sectionName=EPIDEMIOLOGY&topicRef=5266&anchor=H175843968&source=see_link#H175843968
- Baxley, E. G., & Gobbo, R. W. (2004, April 01). Shoulder Dystocia. Retrieved October 9, 2018, from https://www.aafp.org/afp/2004/0401/p1707.html
- Erb’s Palsy. (n.d.). Retrieved October 9, 2018, from https://www.physio-pedia.com/Erb’s_Palsy


