Therapeutic Hypothermia (Cooling Therapy) for Babies with Hypoxic-Ischemic Encephalopathy (HIE)
What is Hypoxic-Ischemic Encephalopathy (HIE)?
Hypoxic-ischemic encephalopathy (HIE) is a type of neonatal brain injury caused by oxygen deprivation and/or limited blood flow to the brain at or near the time of birth. It can result in permanent brain injury, lifelong disabilities such as cerebral palsy (CP), and even infant death.
However, a cutting-edge treatment called therapeutic hypothermia (also referred to as “cooling”) can minimize the risks associated with HIE.
Therapeutic hypothermia is the standard treatment for HIE. It can slow down the injury process, allowing the baby’s brain to heal and minimizing the spread of damage. Clinical evidence has shown that therapeutic hypothermia has benefited full-term infants with moderate to severe HIE.
Did your child receive cooling therapy for HIE?
Tell us your story. Our trusted team is here to help.
What is therapeutic hypothermia?
Therapeutic hypothermia (also known as hypothermia therapy, brain cooling, cooling therapy, or cooling treatment) is a procedure used to help slow down the injury process associated with HIE. While it’s now being used in numerous different fields (e.g. treating heart attacks, strokes, and traumatic injuries in adults), in the context of birth injury, the process focuses specifically on slowing down a baby’s brain injury.
This type of HIE therapy works by cooling the baby to about 92.3 – 94.1 degrees Fahrenheit (33.5 – 34.5 degrees Celsius) for 72 hours, ideally within six hours of birth, or the oxygen-depriving event.
To administer therapeutic hypothermia for HIE, doctors may use either a cooling cap (selective brain cooling) or a cooling blanket (whole body cooling). Either of these methods can be effective; the choice of one or the other depends on the medical institution, and the equipment that is available in that particular NICU.
During the treatment, NICU (neonatal intensive care unit) staff closely monitor the baby’s vital signs like respiration, oxygenation, heart rate, and brain wave activity. Physicians use this data to determine how the baby is responding overall to the cooling treatment.
Following therapeutic hypothermia, the baby is re-warmed slowly (over at least four hours) until they are at 97.7 – 98.6 degrees Fahrenheit (36.5 – 37 degrees Celsius).
How does therapeutic hypothermia work?
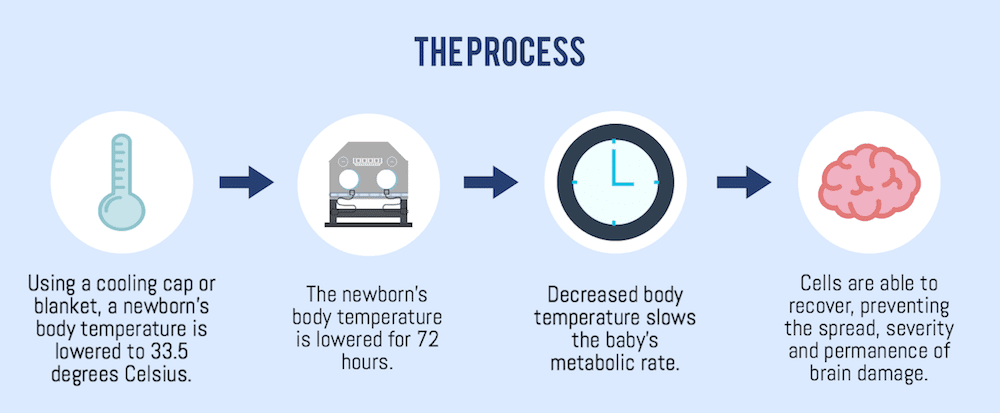
Lowering the body’s temperature slows the metabolic rate and allows cells more time to recover from neurological (brain) damage. This can help reduce the extent of injury, which can potentially improve the baby’s prognosis.
When should doctors perform therapeutic hypothermia?
Guidelines for cooling continue to evolve as research progresses, and exact criteria varies from hospital to hospital. However, in 2016, the Academic Medical Center Patient Safety Organization (AMC PSO) provided the following general recommendations from a task force on neonatal encephalopathy.
Therapeutic hypothermia should be given when all three of the following criteria are met:
1. The baby is less than six hours of age* and was born after at least 36 weeks of pregnancy.
2. At least one of the following occurred:
- A complication before delivery, such as cord prolapse, uterine rupture, or profound fetal bradycardia
- An Apgar score of five or lower at 10 minutes of life
- Prolonged resuscitation at birth
- Severe acidosis (very acidic blood)
- Abnormal base excess within 60 minutes of birth, as shown in umbilical cord gas or neonate blood gas
3. At least one of the following is observed:
- Signs of neonatal seizures
- Evidence of neonatal encephalopathy in a clinical exam
Additionally, physicians are advised to consider administering therapeutic hypothermia when all three of these criteria are met:
1. The baby is no more than 12 hours of age* and was born after at least 34 weeks of pregnancy.
2. At least one of the following occurred:
- A complication before delivery, such as cord prolapse, uterine rupture, or profound fetal bradycardia
- An Apgar score of five or lower at 10 minutes of life
- Prolonged resuscitation at birth
- Acidosis
- Abnormal base excess within 60 minutes of birth, as shown in umbilical cord gas or neonate blood gas
- A collapse after birth that results in hypoxic-ischemic injury.
3. At least one of the following is observed:
- Signs of neonatal seizures
- Evidence of neonatal encephalopathy in a clinical exam
*Recent research indicates that therapeutic hypothermia may still be beneficial when started up to 24 hours after birth, but its effectiveness is not yet proven. The standard is to administer the treatment within 6 hours of birth.
Did your baby receive cooling treatment in time?
Our HIE lawyers advocate relentlessly for children like yours. Contact us to learn about your legal options.
When should a baby not receive therapeutic hypothermia?
The AMC PSO guidelines state that babies should not receive therapeutic hypothermia if they had a premature birth (under 34 weeks into pregnancy), and that physicians should exercise extreme caution if they weigh less than 1,750 grams (3-4 lbs), have severe congenital abnormalities, suffered major intracranial hemorrhage, have overwhelming septicemia, or show evidence for a blood clotting disorder that could make the treatment dangerous.
Current evidence does not support the cooling of babies born before 35 weeks or who have mild hypoxic-ischemic encephalopathy.
Did my baby need brain cooling?
Babies receive cooling therapy when they meet the criteria outlined above. Medical providers may fail to explain to parents why their baby is receiving cooling therapy. This may be because the baby suffered HIE during the perinatal period (while under the hospital’s care), and negligent conduct of the medical providers may have caused the HIE injury. In other words, your child’s injury could have been prevented. It’s beyond upsetting to learn that the people you trusted with your care made a mistake, but fortunately, you are not alone, and there are resources to help you and your child.
If the medical staff did not follow procedure and meet standards of care, that constitutes medical negligence. Medical providers should inform parents whether their baby’s medical condition requires them to receive cooling therapy. Medical staff are responsible for making sure that parents are informed when a baby meets criteria for HIE, and cooling therapy should be given. If your baby met the criteria for cooling and medical staff did not provide cooling therapy to your baby, then they are negligent. You may be entitled to financial compensation for your child’s injuries.
Medical mistakes are a patient safety problem – they often can be prevented, but when proper care is not provided, patients are harmed. It is the duty of medical practitioners to prevent errors from occurring – if they do something that causes the patient harm, it falls squarely into the category of medical malpractice.
How can an attorney help?
If your child was diagnosed with HIE, speak to a birth injury lawyer to see whether your child’s HIE was caused by improper care during pregnancy or during delivery. A favorable verdict or settlement can provide for future care and the lifelong support that your child will need as a result of medical negligence.
Our birth injury attorneys at ABC Law Centers: Birth Injury Lawyers have decades of experience handling cases where brain cooling was administered – either whole-body cooling or head cooling only. We also deal with situations where:
- Brain cooling was needed due to a medical error
- Brain cooling was needed and not administered
- Brain cooling wasn’t administered properly
- Brain cooling wasn’t done quickly enough
- Brain cooling was needed but doctors missed the the signs of HIE
- Brain cooling was undertaken but medical staff didn’t provide adequate supportive treatment
Because brain cooling is a very medically complex topic, it’s important that the lawyer you choose is a birth injury attorney specifically – for example, the field of personal injury is far too vast for a lawyer who does slip-and-fall accidents or medical device malfunctions to be able to give clients who have a child with a birth injury the level of attention they deserve. Our attorneys focus only on birth injury and work with an established network of leading medical, forensic, and economic specialists that consult on every single case.
Birth injury is incredibly personal and we have witnessed firsthand how challenging it can be for any family. We have worked with brave parents like yourself for over 25 years, and it has been our honor to help secure lifetime care for their children. We are privileged to get to know each family and become the advocates they need. When you contact our firm, you will not be a case number to us – we treat every client like family. Contact us at a time convenient for you with any questions you may have. We are here to help you during this challenging time.


About ABC Law Centers: Birth Injury Lawyers
ABC Law Centers: Birth Injury Lawyers is a birth injury law firm focused exclusively on cases involving HIE and other birth injuries. In a birth injury case, settlement money can be used to pay for a child’s lifelong treatment, therapy, and a secure future. If you believe that your child’s HIE may have been caused by a negligent medical professional or hospital, or that your child was not given therapeutic hypothermia when they should have been, you may have a case. Contact us at your convenience to learn more; we can be reached around the clock. We are happy to talk to you free of any charge. In fact, you would pay nothing throughout the entire legal process unless we win your case.
Featured Videos
Posterior Position
Hypoxic-Ischemic Encephalopathy (HIE)

Featured Testimonial
What Our
Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on. ABC Law Centers: Birth Injury Lawyers was just that.
- Michael
Helpful resources
- Davidson, J. O., Wassink, G., van den Heuij, L. G., Bennet, L., & Gunn, A. J. (2015). Therapeutic Hypothermia for Neonatal Hypoxic-Ischemic Encephalopathy – Where to from Here?. Frontiers in neurology, 6, 198. doi:10.3389/fneur.2015.00198
- Shankaran, Seetha, et al. Whole-Body Hypothermia for Neonates with Hypoxic–Ischemic Encephalopathy. N Engl J Med 2005; 353:1574-1584. October 13, 2005. DOI: 10.1056/NEJMcps050929.
- Mosalli R. (2012). Whole body cooling for infants with hypoxic-ischemic encephalopathy. Journal of clinical neonatology, 1(2), 101-6.
- Guillet, R. Seven- to eight-year follow-up of the CoolCap trial of head cooling for neonatal encephalopathy. Pediatr Research 2012 Feb; 71(2):205-9. doi: 10.1038/pr.2011.30. Epub 2011 Dec 21.
- The Academica Medical Center Patient Safety Organization (AMC PSO) Neonatal Encephalopathy Task Force. (2016). Therapeutic Hypothermia in Neonates: Recommendations of the Neonatal Encephalopathy Task Force[Pamphlet].


