Subdural Hemorrhages/Hematomas
Infant intracranial hemorrhages, or brain bleeds, are a type of birth injury that can occur when a baby experiences a traumatic labor and delivery. In this article, we focus specifically on a form of intracranial hemorrhage known as subdural hemorrhages (or subdural hematomas). We’ll review the risk factors for and causes of subdural hemorrhages, how these bleeds are treated, and what parents can expect for their child in the long-term. We will also discuss legal options for parents who suspect that their child’s subdural hemorrhage may have been caused by medical malpractice.
What Is a Subdural Hemorrhage/Hematoma?
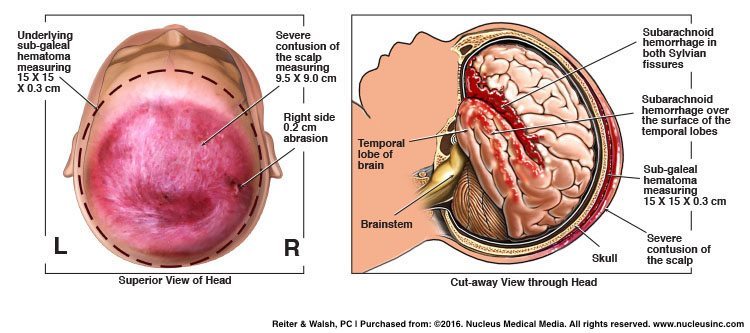
A subdural hemorrhage/hematoma is the most common type of brain bleed in a newborn. This type of bleed occurs when there is rupture of the blood vessels in the area between the surface of the brain and the thin layer of tissue that separates the brain from the skull.
Signs of Subdural Hemorrhages/Hematomas
Signs of a subdural hemorrhage include the following:
- Respiratory depression (slow and/or shallow breathing)
- Apnea (periods of not breathing)
- Seizures
- Irritability
- Altered tone (very limp or very tense)
- Altered level of consciousness
The symptoms of this type of brain bleed usually occur within the first 24 – 48 hours of life. Sometimes a subdural hemorrhage causes an increase in pressure inside the brain, which can cause an increase in head size, apnea, bradycardia (slow heart rate), and coma.
Risk Factors for and Causes of Subdural Hemorrhages/Hematomas
A lack of oxygen to the baby’s brain during or near the time of delivery can place a baby at risk of having a subdural hemorrhage. However, trauma to the head is a more common cause of this type of bleed.
Risk factors for and causes of a subdural hemorrhage include the following:
- Oxygen deprivation/hypoxic-ischemic encephalopathy (HIE)
- Use of forceps or vacuum extractors to facilitate delivery
- A vaginal delivery when the baby is in breech presentation.
- Research shows that a C-section delivery is the safest way to deliver babies in this position.
- Improperly managed brow or face presentation
- Macrosomic (unusually large) baby
- Cephalopelvic disproportion (CPD). This is a situation in which the baby’s head is too large to fit through the mother’s pelvis.
- Precipitous delivery. This is very fast delivery, often accompanied by strong contractions. Drugs used to start or speed up labor and delivery, such as Pitocin (oxytocin) and Cytotec, can cause contractions that are so fast and strong that they deprive the baby of oxygen. Sometimes strong contractions can also cause head trauma.
- Prolonged labor and delivery. Prolonged labor can be very traumatic for a number of reasons. Labor in general is stressful for a baby due to the repeated force of contractions on the baby’s head. Trauma can occur when a baby is very large, when the baby is not in the normal position in the birth canal, or in cases of cephalopelvic disproportion. Many conditions can cause prolonged labor, and oftentimes, physicians fail to move on to C-section delivery when it is medically necessary. During the extended vaginal labor and attempted delivery, the physician may use Pitocin or Cytotec to try and speed up delivery, or vacuum extractors and forceps may be used to try and facilitate delivery. All of these actions can cause a traumatic injury to the head with resultant brain bleeding.
Diagnosis of Subdural Hemorrhages/Hematomas
A CT (computed tomography) of the head is the best way to diagnose a subdural hemorrhage. Some babies have no symptoms, which is why it is crucial for the medical team to closely monitor all babies who had a traumatic birth and who are suspected of having this type of brain bleed. Of course, management of a subdural hematoma should begin right away. A low blood volume (hypovolemia) and low blood pressure can cause the baby to go into hypovolemic shock, which can lead to hypoxic-ischemic encephalopathy (HIE).
Treatment of Subdural Hemorrhages/Hematomas
Treatment and management of a subdural hemorrhage depends on the location and extent of the bleed. The baby should have frequent hematocrit (red blood cell) testing to assess ongoing blood loss. When there is significant blood loss that causes hypovolemia, normal saline should be given to increase the baby’s blood volume and blood pressure, followed by whole blood transfusion. If the baby is having seizures, antiepileptic drug therapy should be initiated, in most cases. If the baby has increased intracranial pressure (ICP), they may need to have surgical removal of the blood.


ABC Law Centers: Birth Injury Lawyers: Birth Injury and Neonatal Brain Bleed Attorneys
Brain bleeds in a baby are very serious and can cause permanent brain injury and lifelong conditions such as cerebral palsy (CP), developmental delays, and seizure disorders.
If you believe that your child or loved one may be experiencing serious consequences of a subdural hemorrhage, the award-winning attorneys at ABC Law Centers: Birth Injury Lawyers can assist. We have helped children throughout the country obtain compensation for lifelong treatment, therapy, and a secure future, and we give personal attention to each child and family we represent. Our firm has numerous multi-million dollar verdicts and settlements that attest to our success, and no fees are ever paid to our firm until we win your case.
Featured Videos
Posterior Position
Hypoxic-Ischemic Encephalopathy (HIE)

Featured Testimonial
What Our
Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on. ABC Law Centers: Birth Injury Lawyers was just that.
- Michael
Helpful resources
- McKee-Garrett TM. Neonatal birth injuries.In: UpToDate. Kim MS (Ed), UpToDate, Waltham, MA, 2014.
- Whitby EH, Griffiths PD, Rutter S, et al. Frequency and natural history of subdural haemorrhages in babies and relation to obstetric factors. Lancet 2004; 363:846.
- Chamnanvanakij S, Rollins N, Perlman JM. Subdural hematoma in term infants. Pediatr Neurol 2002; 26:301.
- Looney CB, Smith JK, Merck LH, et al. Intracranial hemorrhage in asymptomatic neonates: prevalence on MR images and relationship to obstetric and neonatal risk factors. Radiology 2007; 242:535.
- Demissie K, Rhoads GG, Smulian JC, et al. Operative vaginal delivery and neonatal and infant adverse outcomes: population based retrospective analysis. BMJ 2004; 329:24.
- Boulet SL, Alexander GR, Salihu HM, Pass M. Macrosomic births in the united states: determinants, outcomes, and proposed grades of risk. Am J Obstet Gynecol 2003; 188:1372.
- Nassar AH, Usta IM, Khalil AM, et al. Fetal macrosomia (> or =4500 g): perinatal outcome of 231 cases according to the mode of delivery. J Perinatol 2003; 23:136.
- Moczygemba CK, Paramsothy P, Meikle S, et al. Route of delivery and neonatal birth trauma. Am J Obstet Gynecol 2010; 202:361.e1.


