Intrauterine Growth Restriction (IUGR)
Intrauterine growth restriction (IUGR) is a condition in which an unborn baby’s growth is too slow. IUGR is sometimes called fetal growth restriction (FGR) or small for gestational age (SGA).
IUGR can be caused by problems with the placenta or uterus, as well as underlying maternal or fetal health issues (1). Certain risk factors and physical examination results help doctors suspect IUGR prenatally; it can then be diagnosed by ultrasound (2).
Babies with IUGR need to be delivered early because they typically do not tolerate contractions or labor well. Because IUGR is such a dangerous condition, failure to diagnose it and recommend an early delivery constitutes medical malpractice.
Babies that have IUGR are at risk of the following:
- Hypoxic ischemic encephalopathy (HIE)
- Brain damage
- Cerebral palsy
- Seizure disorders
- Intellectual disabilities
- Developmental delays
- Fetal acidosis
Risk Factors and Causes of Intrauterine Growth Restriction (IUGR)
There are a variety of factors related to the placenta/uterus, maternal health, or fetal health that can lead to IUGR. Causes and risk factors for IUGR include the following (5):
Placental/Uterine Factors:
- Placental abruption: This is when the placenta separates, either completely or partially, from the wall of the uterus before the baby is born. Partial placental abruption can cause IUGR.
- Infection of the tissues: that surround the growing baby (see chorioamnionitis).
- Decreased blood and nutrient flow in the uterus and/or placenta.
Maternal Factors:
- Maternal high blood pressure/preeclampsia
- Diabetes
- Maternal heart issues
- Maternal kidney diseases
- Maternal infection
- Malnutrition
- Anemia
- Small mother and parents
- Poor weight gain in pregnancy
- Mother weighs less than 100 lbs at the start of pregnancy
- Use of cigarettes during pregnancy
Fetal Factors:
- Fetal infection
- Multiples pregnancy (twins or more)
- Genetic issues
Please note that this is not a complete list. For more risk factors and causes, please click here.
Detecting and Diagnosing Intrauterine Growth Restriction (IUGR)
IUGR has been diagnosed using both ultrasound examinations and fundal height measurements. Fundal height is measured during a routine prenatal exam. The fundal height (distance from the pubic bone to the top of the uterus) may suggest the baby is too small for the gestational age.
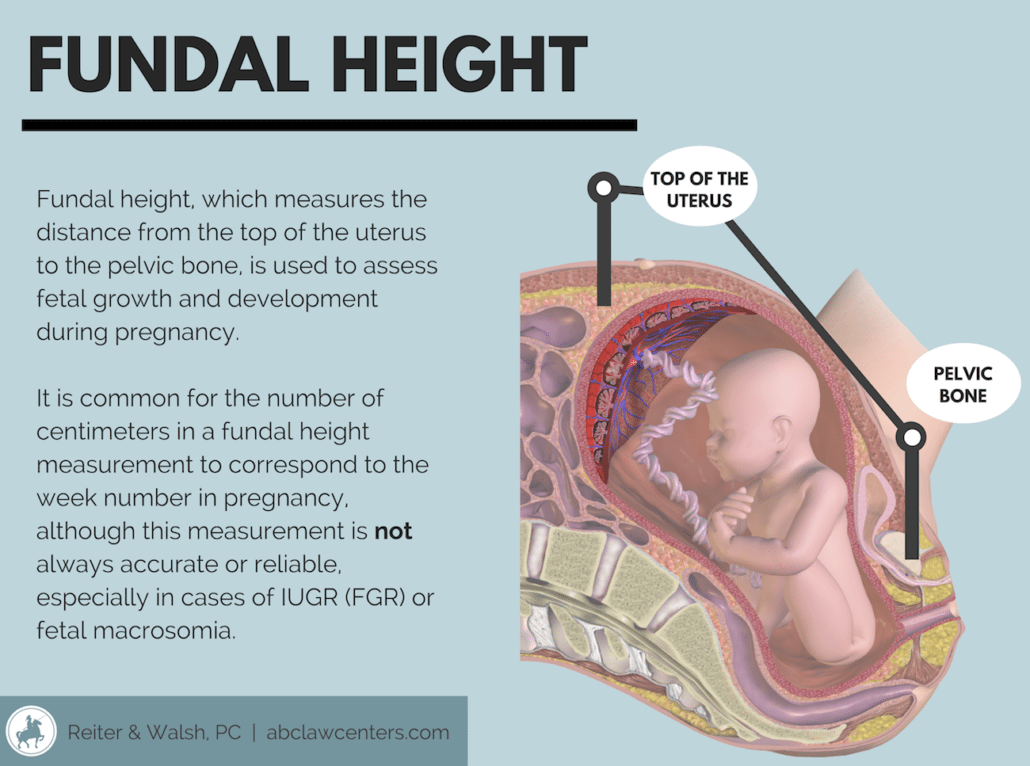
The fundal height measurement can be inaccurate, so standard of care requires other testing to make sure the baby has a healthy development.
Ultrasound
The main test for checking a baby’s growth in the womb is an ultrasound, which involves using sound waves to create pictures of the baby. Ultrasound can be used to measure the baby’s head and abdomen. The doctor can compare those measurements to growth charts to estimate the baby’s weight. An ultrasound is accurate in diagnosing FGR about 80 – 90% of the time. The test can also be used to determine how much amniotic fluid is in the womb. A low amount of amniotic fluid (oligohydramnios) could indicate FGR.
Doppler Flow
Doppler flow uses sound waves to measure the amount and speed of blood flow through the blood vessels. This test is sometimes used to check the flow of blood in the umbilical cord and vessels of the uteroplacental circulation.
Weight checks. The mother’s weight is checked at every prenatal visit. If a mother is not gaining weight, it could indicate a growth problem in the baby.
Amniocentesis
This is a procedure where a needle is inserted through the mother’s abdomen and into her uterus to withdraw a small amount of amniotic fluid for testing. Tests may detect infection or some chromosomal abnormalities that could lead to FGR.
Fetal Monitoring
The physician will initiate a regular schedule of prenatal tests up through the time of delivery. These tests typically include weekly nonstress tests, biophysical profiles and serial ultrasounds to assess the baby’s heart rate in response to her movement, level of amniotic fluid and to determine the level of fetal growth.
Management of IUGR
Upon receiving an IUGR diagnosis, the mother may be referred to maternal-fetal specialists. These are physicians with specialized training and expertise in the management of IUGR. They should very carefully monitor the baby’s health throughout the remainder of the pregnancy.
There are a variety of tests that should be done to assess the wellbeing of a baby with IUGR. These include the following:
- Weight checks. Medical staff should check the mother’s weight at each prenatal visit. If a mother is not gaining weight, this should prompt doctors to check for a fetal growth problem (9).
- Non-stress tests (NSTs). The non-stress test is a simple test performed to ensure that unborn babies’ hearts react appropriately to different forms of movement and stimulation.
- Amniotic fluid index (AFI). An ultrasound can obtain a measurement called the amniotic fluid index, or AFI. This can reveal if there is oligohydramnios (abnormally low amniotic fluid) or polyhydramnios (abnormally high amniotic fluid).
- Biophysical profiles (BPP). The biophysical profile (BPP) predicts the presence or absence of fetal asphyxia (severe hypoxia) as well as the risk of death during the antenatal period (the short period after birth).
- Doppler velocimetry. Doppler velocimetry is a prenatal test that gives physicians information about uteroplacental blood flow and the baby’s responses to physiological challenges.
If the findings of these studies are non-reassuring, prompt delivery needs to be considered.
Timing of Delivery for IUGR During Pregnancy
Because of the extreme risk associated with moderate to severe fetal IUGR, many physicians will recommend early delivery.
Treatment for IUGR, based on gestational age, includes the following:
- If the pregnancy is 34+ weeks along, physicians may recommend an early delivery (often via c-section).
- If the pregnancy is less than 34 weeks along, physicians will continue to carefully monitor the health of the fetus and the amount of amniotic fluid. If the believe the baby is in serious danger, they will recommend an early delivery. They must weigh the risks of prematurity with the risks of IUGR-associated complications. When delivery is suggested prior to 34 weeks, the physician may recommend an amniocentesis to help evaluate fetal lung maturity. This can help determine how likely a baby is to suffer from respiratory distress syndrome or other issues. If the lungs are underdeveloped, physicians may also recommend certain treatments that can help accelerate development in utero or improve breathing once the baby is born (10).
- In any case, delivery must occur before 40 weeks gestation.
Dangers of IUGR
Small babies do not tolerate contractions or labor well. As such, they can be deprived of oxygen and may experience a number of complications. These include the following:
- Meconium passage
- Hypoglycemia
- Polycythemia
- Problems with thermoregulation
- Hypoxic-ischemic encephalopathy (HIE)
- Cerebral palsy (CP)
- Brain bleeds
- Periventricular leukomalacia (PVL)
- Necrotizing enterocolitis
- Sepsis
- Death
Intrauterine Growth Restriction (IUGR) and Medical Malpractice
When risk factors for IUGR are present or when IUGR is confirmed during pregnancy, it is essential that the physician properly assess and monitor the growth of the baby. In certain instances, it may be necessary to plan to deliver the baby early. Failure to treat the underlying cause of the IUGR and to properly monitor and plan for the birth can result in serious and permanent injuries. If this happens, it constitutes medical malpractice.


Get Legal Help for Your Family: ABC Law Centers: Birth Injury Lawyers
At ABC Law Centers: Birth Injury Lawyers, we work closely with a network of trustworthy attorneys across the country. Our attorneys focus exclusively on birth injury cases. We can share our knowledge on the complicated medical aspects of these cases and provide the compassion each family needs during this difficult time. Our staff is always available to answer any questions parents and caretakers may have.
Featured Videos
Posterior Position
Hypoxic-Ischemic Encephalopathy (HIE)

Featured Testimonial
What Our
Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on. ABC Law Centers: Birth Injury Lawyers was just that.
- Michael
Helpful resources
- (n.d.). Retrieved August 23, 2018, from https://www.uptodate.com/contents/infants-with-fetal-intrauterine-growth-restriction
- (n.d.). Retrieved August 23, 2018, from https://www.uptodate.com/contents/fetal-growth-restriction-diagnosis?topicRef=5062&source=see_link
- Intensive Care Nursery House Staff Manual: Intrauterine Growth Retardation[PDF]. (2004). San Francisco: UCSF Children’s Hospital.
- O’Connor, H., Unterscheider, J., Daly, S., Geary, M., Kennelly, M., McAuliffe, F., … & Dicker, P. (2015). 321: Comparison of asymmetric versus symmetric IUGR–results from a national prospective trial. American Journal of Obstetrics & Gynecology, 212(1), S173-S174.
- Default – Stanford Children’s Health. (n.d.). Retrieved August 23, 2018, from https://www.stanfordchildrens.org/en/topic/default?id=intrauterine-growth-restriction-iugr-90-P02462
- American College of Obstetricians and Gynecologists. (2013). ACOG Practice bulletin no. 134: fetal growth restriction. Obstetrics and gynecology, 121(5), 1122.
- Moh, W., Graham, J. M., Wadhawan, I., & Sanchez-Lara, P. A. (2012). Extrinsic factors influencing fetal deformations and intrauterine growth restriction. Journal of pregnancy, 2012.
- Gutaj, P., & Wender-Ozegowska, E. (2016). Diagnosis and management of IUGR in pregnancy complicated by type 1 diabetes mellitus. Current diabetes reports, 16(5), 39.
- Strauss, R. S., & Dietz, W. H. (1999). Low maternal weight gain in the second or third trimester increases the risk for intrauterine growth retardation. The journal of nutrition, 129(5), 988-993.
- Intrauterine growth restriction | Small for Gestational Age. (2017, February 22). Retrieved August 23, 2018, from http://americanpregnancy.org/pregnancy-complications/intrauterine-growth-restriction/


