Placenta Accreta
Placenta Accreta, Birth Injury, and Medical Malpractice
Placenta accreta is a condition in which the placenta does not properly separate from the uterus during labor and delivery because it has grown too deeply into the uterine wall (1). This condition is usually diagnosed during a routine prenatal ultrasound. If undetected and not properly treated, placenta accreta can cause severe hemorrhages, which can pose a serious health threat to both mother and child.
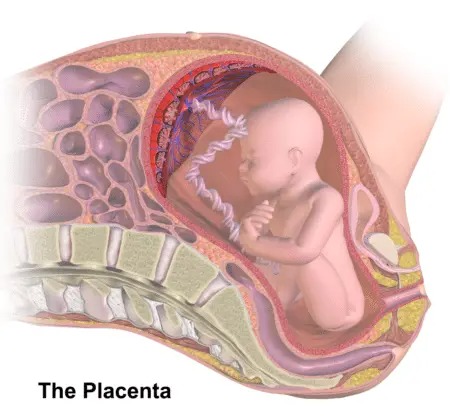
What is the placenta?
The placenta is an organ that transports oxygen and nutrients from the mother to the baby and removes waste from the baby during pregnancy. In a normal pregnancy, the placenta is attached to the wall of the uterus until birth. Once the baby is delivered, the placenta then naturally separates from the uterine wall and leaves the body through the birth canal in the period called afterbirth (2). Sometimes, however, the placenta is unable to detach properly because it is too deeply attached to the uterine wall. There are three complications in which the placenta becomes too deeply attached. These include placenta accreta (when the placenta attaches too deeply to the uterine wall), placenta increta (when the placenta penetrates the uterine wall and attaches to the uterine muscle), and placenta percreta (when the placenta pushes through the uterine wall entirely and attaches to a different organ). Roughly 1 in 2,500 pregnancies experiences one of these placental conditions.
Placenta accreta is the most common of the three attachment complications, and it occurs in 75% of cases of abnormal placental attachment (1). Placenta accreta is a serious complication, as it can cause severe blood loss, which can impact the health of both mother and child.
Signs of placenta accreta
Many women with placenta accreta do not experience any signs or symptoms. However, women may experience bleeding during pregnancy, especially during their third trimester. If you experience any bleeding during your pregnancy, please consult with a medical professional immediately. It is critical that medical personnel detect, diagnose, and properly manage any bleeding during pregnancy.
Placenta accreta is usually diagnosed during the prenatal period when medical practitioners conduct routine ultrasounds (1). For this reason, it is imperative that medical professionals administer ultrasounds on a regular basis and interpret them meticulously. Additionally, if the doctor suspects placental complications, but is not certain, they may request a magnetic resonance imaging (MRI) be done as an adjunctive diagnostic tool (4).
Risk factors for placenta accreta
Women are more likely to develop placenta accreta if they have experienced:
- Multiple pregnancy (a pregnancy with more than one baby)
- Advanced maternal age (pregnancy over the age of 35)
- Previous uterine surgery
- Previous cesarean deliveries
- Previous births (the chances of developing placenta accreta increase with the number of times a woman gives birth) (4)
- Placental placement issues like placenta previa (if the placenta partially or completely covers the cervix or sits lower in the uterus, the risk of placenta accreta increases) (4)
Risks and complications associated with placenta accreta: the mother
Under normal circumstances, the placenta will separate from the uterine wall completely during a vaginal delivery. In placenta accreta, this separation can cause heavy bleeding, or hemorrhaging, in the mother. Hemorrhages can cause life-threatening blood loss and severe drops in blood pressure (1).
Hemorrhaging in the mother can also lead to other complications, including disseminated intravascular coagulopathy (the inability for the blood to clot normally), kidney failure, lung failure, or the need for a blood transfusion (4).
Risks and complications associated with placenta accreta: the baby
Placenta accreta can cause labor to begin early, resulting in premature delivery, which can cause myriad complications for the baby (4). These can include hypoxic ischemic encephalopathy (HIE), cystic periventricular leukomalacia (PVL), intracranial hemorrhages, and other injuries. Because of this, it is crucial that medical personnel detect, diagnose, and properly manage placenta accreta on prenatal ultrasound. Once placenta accreta is diagnosed, the doctor will be able to recommend ways of managing the pregnancy to prepare for any risks and complications.
Premature babies may be at risk for hypoxic-ischemic encephalopathy (HIE), which is a brain injury caused by oxygen deprivation. Premature birth and HIE both increase the risk that a baby will develop cerebral palsy, which is a group of non-progressive motor conditions that cause physical disability.
Management of placenta accreta
In general, the management of placenta accreta involves diagnosing the condition during the prenatal period (4). The doctor will then focus on managing the condition by trying to get the patient to term and monitoring the baby very closely along the way. The condition will usually be managed with a planned cesarean delivery with an experienced surgical team equipped to remove the placenta and vessels from the uterine wall. In certain instances, removal of the placenta may be combined with a hysterectomy. The medical professionals will be able to devise a plan for delivery which will optimize outcomes for both the mother and the baby.
Hysterectomy
Placenta accreta is a common indication for a hysterectomy, or the full removal of the uterus, to prevent or control hemorrhage (3). If a hysterectomy is necessary, the doctors will remove the uterus with the placenta still attached during a cesarean delivery (4). It is important to note that, after a hysterectomy, the patient will not be able to get pregnant again.
Adverse outcomes are often preventable. If the physician fails to appropriately diagnose and treat placenta accreta, based on clinical findings and ultrasound screening, he or she may not be providing the care required by law. Failure to match the standard of care when presented with certain clinical findings is medical malpractice.
Disclaimer: This page is intended solely as an educational tool for parents. It is not intended as, and should not be mistaken for, medical advice. If you have any medical concerns about your pregnancy, such as abnormal bleeding, please seek medical attention immediately. Bleeding during pregnancy is a condition that must be evaluated and treated by a medical professional.


Legal help for birth injuries from mismanaged placenta accreta
The award-winning attorneys at ABC Law Centers: Birth Injury Lawyers have helped dozens of children affected by birth injuries such as hypoxic-ischemic encephalopathy (HIE) and cerebral palsy. Our firm is based in Detroit, Michigan, but we handle cases all over the U.S.
Please contact us today to learn more. Our birth injury attorneys are available to speak with you 24/7, and there is no fee unless we win your case.
Featured Videos
Posterior Position
Hypoxic-Ischemic Encephalopathy (HIE)

Featured Testimonial
What Our
Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on. ABC Law Centers: Birth Injury Lawyers was just that.
- Michael
Helpful resources
- Placenta Accreta: Symptoms, Risks and Treatment. (2017, April 04). Retrieved January 30, 2019, from http://americanpregnancy.org/pregnancy-complications/placenta-accreta/
- Placental accreta, increta and percreta. (n.d.). Retrieved January 30, 2019, from https://www.marchofdimes.org/complications/placental-accreta-increta-and-percreta.aspx
- Resnik, R., & Silver, R. (n.d.). Clinical features and diagnosis of placenta accreta spectrum (placenta accreta, increta, and percreta). Retrieved January 30, 2019, from https://www.uptodate.com/contents/clinical-features-and-diagnosis-of-placenta-accreta-spectrum-placenta-accreta-increta-and-percreta
- Placenta accreta. (2018, June 05). Retrieved January 30, 2019, from https://www.mayoclinic.org/diseases-conditions/placenta-accreta/symptoms-causes/syc-20376431


