Oligohydramnios (Low Amniotic Fluid)
What is oligohydramnios?
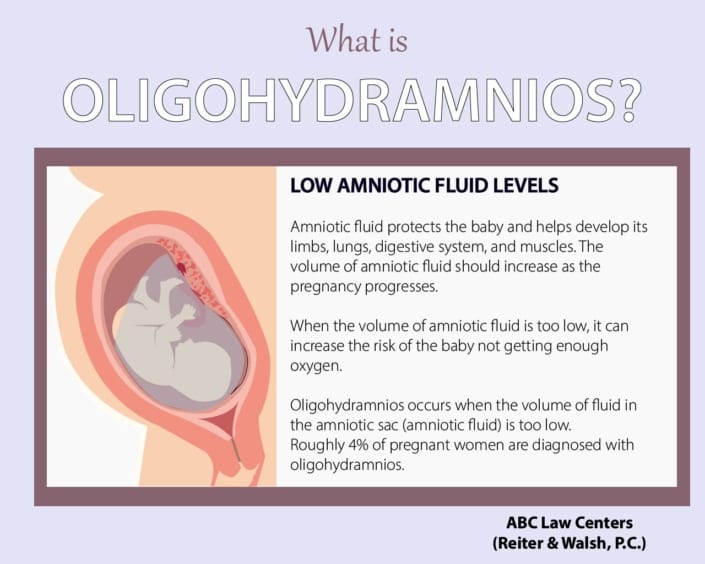
Oligohydramnios occurs when the amniotic fluid level is too low. Amniotic fluid is a protective barrier surrounding a baby in the amniotic sac, or womb. Roughly 4% of pregnant women are diagnosed with oligohydramnios.
What is amniotic fluid?
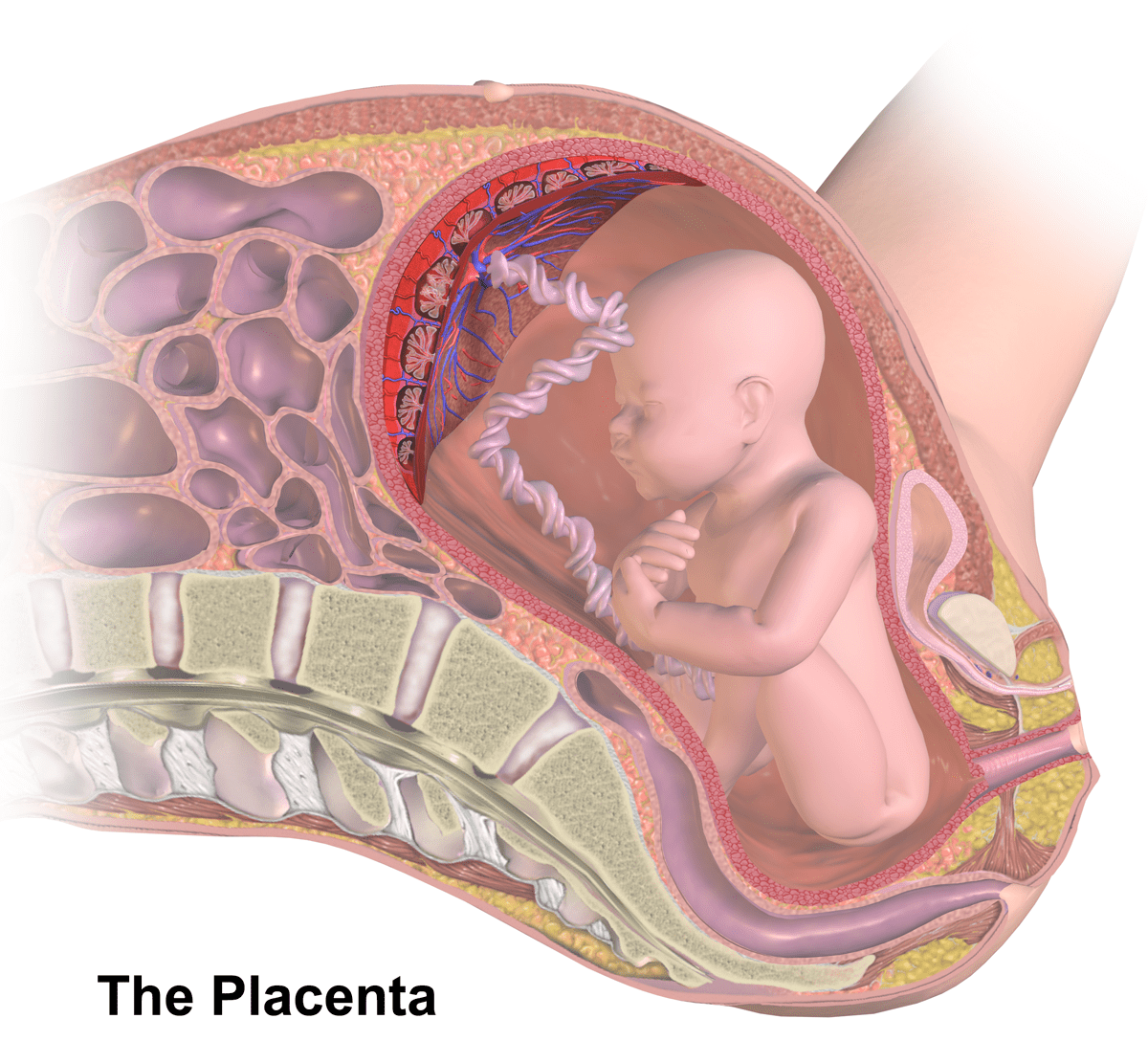
Amniotic fluid is the liquid that surrounds the fetus during pregnancy. Located in the amniotic sac (the womb), amniotic fluid protects and provides nutrients to the developing baby that help it mature, grow, and maintain a consistent body temperature. Amniotic fluid also provides a cushion around the baby and umbilical cord to prevent injuries like cord compression and oxygen deprivation.
At the earliest stage of development, amniotic fluid consists mainly of water. At approximately 20 weeks, the baby’s urine becomes the primary substance. The baby “breathes” and swallows amniotic fluid. The volume of amniotic fluid increases as the pregnancy progresses and reaches its peak at about 34 weeks. Oligohydramnios, a decrease in the levels of amniotic fluid, is a serious health risk to the baby.
What causes oligohydramnios?
Oligohydramnios can occur any time during pregnancy, but is most commonly diagnosed in the third trimester. Oligohydramnios is typically caused by:
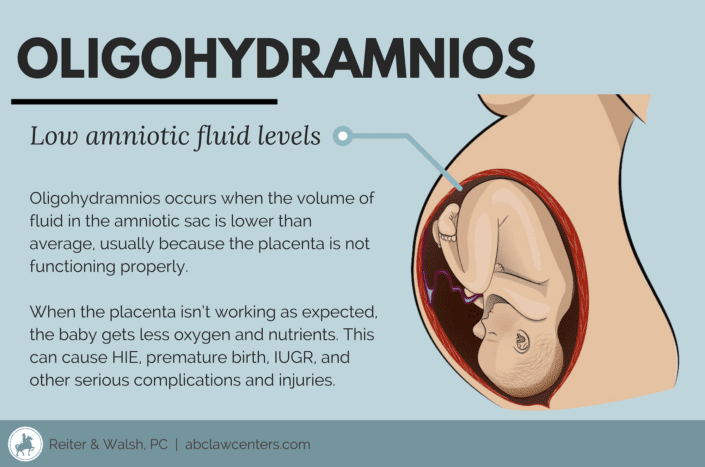
- Placental issues: If the placenta isn’t providing enough nutrients for the baby, then the baby may stop recycling fluid, therefore lowering the amniotic fluid.
- Birth defects: Certain birth defects cause problems in the fetal urinary tract and kidneys, leading to insufficient urine production.
- Premature rupture of membranes (PROM): When the water breaks before labor begins.
- Leaking of amniotic fluid: A tear in the membrane can cause amniotic fluid to leak.
- Post-date pregnancy: A pregnancy that surpasses 40 weeks is at risk of oligohydramnios because the amniotic fluid can decrease by half after this time.
- Maternal problems: Maternal conditions, such as diabetes, dehydration, hypertension, and preeclampsia can impact amniotic fluid levels.
Risk factors for oligohydramnios
In some cases, women who develop oligohydramnios have no identifiable risk factors, which is why physicians must monitor amniotic fluid levels throughout pregnancy. However, many pregnant women do have risk factors for oligohydramnios.
Risk factors for oligohydramnios may include:
- Maternal hypertension/preeclampsia
- Maternal diabetes
- Maternal dehydration
- Maternal hypoxia
- Placental issues
Placental complications can cause oligohydramnios.
Signs and symptoms of oligohydramnios
While they vary, some of the most common signs and symptoms of a lowered amniotic fluid volume are:
- Leaking of the amniotic fluid
- Low amniotic fluid on an ultrasound
- Baby is smaller than what is normal for gestational age (IUGR)
- Low maternal weight gain
- Preterm premature rupture of membranes (PPROM)
- Abdominal discomfort
- Sudden drop in fetal heart rate
- Little to no fetal movement, or decreasing fetal movement
- Abnormal findings on a fetal monitor, including fetal distress
Oligohydramnios is typically diagnosed by:
- A finding in a routine ultrasound
- An ultrasound given to test amniotic fluid level in someone who is at risk
- An ultrasound given in response to a uterine size that is less than expected for gestational age
- An ultrasound given in response to a patient who presents with premature rupture of membranes (PROM)
Ultrasonic diagnosis of oligohydramnios is performed by obtaining a measurement called the amniotic fluid index (AFI). The assessment of amniotic fluid may be used in conjunction with the biophysical profile (BPP) and non-stress test (NST) as part of an assessment of fetal well being. AFI is calculated by measuring the depth of the amniotic fluid in four sections of the uterus and adding them together. The doctor can take objective measurements using the AFI, and will diagnose oligohydramnios when the amniotic fluid index is less than 5 and the single deepest pocket is less than 2 cm. The doctor can also use a dye-dilution method to quantify the volume of amniotic fluid. The doctor must also look at downward trends in amniotic fluid over time.
An AFI less than 5 centimeters indicates oligohydramnios. A borderline AFI of 5-10 centimeters, however, has been associated with many risks, including:
- Fetal heart rate deceleration
- Meconium aspiration
- Low Apgar score
- Low birth weight
- NICU admission
- Non-reactive non-stress tests
- Need for cesarean delivery
Most women with a high-risk pregnancy should have an AFI assessment once a week to monitor for oligohydramnios. Twice-weekly AFI assessments are justified if measurements are between 5 and 10 centimeters at a gestational age of fewer than 41 weeks.
Anyone at 41 weeks of gestation or higher should have twice-weekly AFI assessments with a modified BPP. However, the frequency of testing should be based on the clinical circumstances of each person; the more unstable the maternal or fetal condition, the more frequent the testing.
Research indicates that all pregnant patients diagnosed with oligohydramnios should undergo a non-stress test (NST) and AFI or BPP once or twice weekly until delivery depending on the maternal and fetal condition, especially in cases in which the cause of the condition is unknown. Oligohydramnios must be identified and managed early to prevent the possibility of permanent brain injury to the baby.
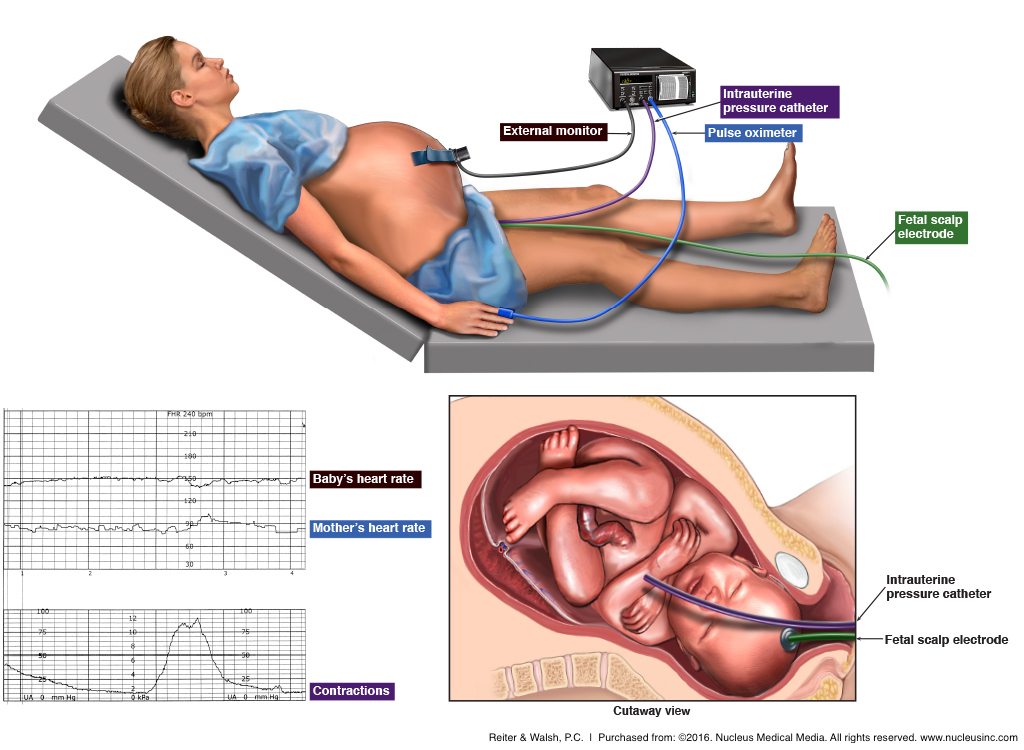
Abnormal findings on a fetal monitor (such as fetal distress) can indicate oligohydramnios
Complications of oligohydramnios
Oligohydramnios can cause the following injuries and complications:
- Increased risk of miscarriage or stillbirth
- Compression of fetal organs that can lead to birth asphyxia or hypoxic-ischemic encephalopathy (HIE)
- Premature birth
- Intrauterine growth restriction (IUGR)
- Cord prolapse
- Cerebral palsy
- Preterm birth
- Meconium aspiration
Managing oligohydramnios throughout pregnancy
Can you increase amniotic fluid levels?
There is no long-term treatment for oligohydramnios. However, a few things can temporarily increase amniotic fluid levels:
- Oral intake of fluids: Some medical professionals may advise patients to stay hydrated if they have oligohydramnios. Oral hydration is simplest, but in some cases, intravenous hydration (through an IV) may be needed.
- Installation of a saline solution into the amniotic sac (amnioinfusion) during labor. During amnioinfusion, doctors use an intra-amniotic catheter to add more liquid to the amniotic fluid. This may help “pad” the umbilical cord, reducing the risks of umbilical cord compression, which could cut off oxygen flow to the baby.
- Investigational therapies: Certain investigational therapies are used to increase amniotic fluid, including tissue sealants, a combination of hydration and DDAVP (desmopressin), and other methods.
It is important to note that the above techniques, even if successful, are temporary. They do not treat the underlying cause of oligohydramnios. In many cases, oligohydramnios can indicate issues with the uteroplacental circulation. In situations where the baby’s circulation may be compromised, the baby may need to be delivered in order to receive treatment.
Managing oligohydramnios during the first trimester
Reduced amniotic fluid during the first trimester is a rare finding, and information regarding the causes of this diagnosis are equally rare. Serial ultrasounds are helpful for following the natural history of the pregnancy, and they help to generate a plan for the care of the condition following the diagnosis.
Managing oligohydramnios during the second trimester
Second trimester oligohydramnios diagnosis can result from fetal or maternal issues. Some fetal disorders may be present, such as intrinsic renal disorders, obstructive lesions in the urinary tract, and other fetal kidney/urinary tract issues. Maternal issues that can cause second trimester oligohydramnios include placental issues, rupture of fetal membranes, and others.
Management and prognosis of oligohydramnios during the second trimester depends on the cause and severity of lowered amniotic fluid volume. In amniotic fluid levels that border on normal, the prognosis is typically positive. Medical professionals usually recommend serial ultrasounds to determine if the condition is stable, resolved, or has progressed into more severe oligohydramnios or fetal growth restriction. More severe oligohydramnios in the second trimester may cause fetal complications or pregnancy loss.
Managing oligohydramnios during the third trimester
Cases of oligohydramnios during the third trimester are often caused by maternal conditions, such as hypertension, preeclampsia, or maternal vascular diseases. These conditions are sometimes related to preterm premature rupture of membranes (PPROM) or uteroplacental insufficiency.
Third trimester oligohydramnios can result in serious injury to the baby. Due to this risk, pregnant patients with oligohydramnios should be closely monitored in a hospital setting and delivered in time when there is fetal distress.
The longer the duration of oligohydramnios, the higher the risk of death and injury to the infant. Physicians typically expect favorable outcomes when they know what is causing lowered amniotic fluid levels and when the baby is being carefully monitored. Whether the cause of oligohydramnios is known or unknown, fetal testing and monitoring may lead to a recommendation for delivery, especially C-section delivery. Standards of care require physicians to discuss the risks and benefits of various management plans with their patients.
Managing oligohydramnios in post-term pregnancies
Amniotic fluid normally decreases post-term, so oligohydramnios is common. Oligohydramnios in post-term pregnancies is associated with higher incidence of meconium-stained fluid and an increased need for C-section delivery. Medical personnel must utilize continuous fetal heart rate monitoring in a hospital setting. If the fetal heart rate becomes abnormal, delivery should occur right away to prevent birth injuries. Monitoring the baby post-term is crucial.
Oligohydramnios and medical malpractice
Improperly managed oligohydramnios can have devastating health consequences for the baby. Therefore, it is essential that physicians follow standards of care and carefully monitor the mother and baby during pregnancy, particularly when risk factors for oligohydramnios are present.
Some areas that may constitute medical negligence in the management or treatment of oligohydramnios include:
- Failure to obtain a thorough history of the mother, thereby missing risk factors for lowered amniotic fluid levels
- Failure to properly monitor the mother and baby during pregnancy and recognize low amniotic fluid, decreasing amniotic fluid, placental insufficiency, fetal distress, or other risk factors for the condition
- Failure to prevent conditions that can cause decreased amniotic fluid volume, such as gestational diabetes, dehydration, chronically high blood pressure, and use of ACE inhibitors
- Failure to follow standards of care regarding timely delivery of the baby, including failure to order and/or perform a timely delivery
- Failure to obtain adequate informed consent from the mother regarding the risks, benefits, and alternatives of various methods of treatment pertaining to amniotic fluid deficiency and associated delivery
Babies with injuries resulting from oligohydramnios often go on to live with permanent disabilities and complex health problems. If a medical professional fails to properly handle decreased amniotic fluid levels and the result is injury, it is considered medical negligence.


Legal help
Children with birth injuries often go on to require expensive, specialized health and lifestyle supports. If you feel your pregnancy was managed improperly and this caused your baby to sustain an injury, contact our birth injury attorneys at ABC Law Centers: Birth Injury Lawyers. Our firm focuses only on birth injury cases, and our clients do not pay anything unless we win or settle their case in their favor.
If you’d like to speak to us regarding your case, please know that your information will always be 100% confidential.
Featured Videos
Posterior Position
Hypoxic-Ischemic Encephalopathy (HIE)

Featured Testimonial
What Our
Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on. ABC Law Centers: Birth Injury Lawyers was just that.
- Michael
Helpful resources
- Low Amniotic Fluid Levels: Oligohydramnios: Causes & Treatment.
- Oligohydramnios: Etiology, diagnosis, and management
- Marchofdimes: Oligohydramnios
- What to Expect: Low Amniotic Fluid (Oligohydramnios) During Pregnancy
- Asgharnia, M., Faraji, R., Salamat, F., Ashrafkhani, B., Dalil Heirati, S. F., & Naimian, S. (2013). Perinatal outcomes of pregnancies with borderline versus normal amniotic fluid index. Iranian journal of reproductive medicine, 11(9), 705-10.


