Macrosomia and Birth Injury
What is macrosomia?
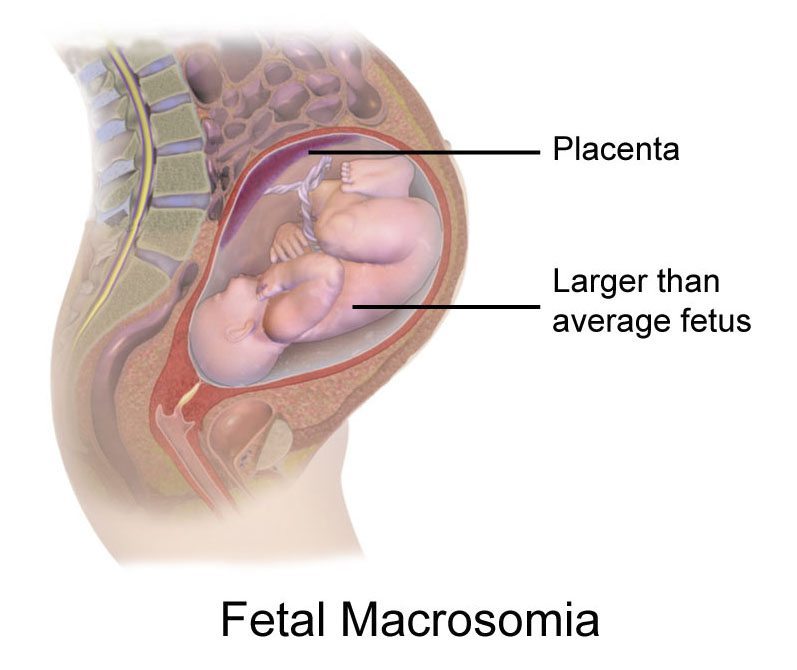
Macrosomia is when an unborn baby is larger than average for their gestational age (how far along the pregnancy is). Babies who are larger than average are referred to as macrosomic.
Fetal macrosomia makes a pregnancy high risk. Macrosomia is associated with/caused by issues such as maternal obesity and gestational diabetes; these are also high-risk pregnancy conditions.
One of the major problems with macrosomia is that the baby may not be able to safely fit through the mother’s pelvis, which can lead to obstetric trauma (injury to the mother), birth trauma (blunt force injury to the baby), and birth asphyxia (fetal oxygen deprivation).
It is imperative that physicians do what they can to prevent macrosomia, which means carefully monitoring maternal health and intervening if necessary (e.g. suggesting strategies to manage diabetes). If a baby becomes macrosomic, it is very important that this condition is diagnosed prenatally so that the timing and management of birth can be planned. In some cases, a C-section will be necessary in order to avoid the dangers associated with vaginal delivery of a macrosomic baby.
Injuries stemming from mismanagement of macrosomia can cause the baby to develop permanent disabilities such as hypoxic-ischemic encephalopathy (HIE), cerebral palsy (CP), and seizure disorders.
How is fetal macrosomia defined?
Macrosomia, also known as large for gestational age (LGA), can be defined as a condition in which a fetus or newborn weighs more than 4,000 grams at term, although some experts use a threshold of 4,500 grams. Researchers have suggested the following grading system, which may be useful for making decisions regarding method of delivery, such as whether to use forceps or vacuum extractors, or whether to perform a C-section (1):
- Macrosomia grade 1: 4,000 – 4,499 grams
- Macrosomia grade 2: 4,500 – 4,999 grams
- Macrosomia grade 3: over 5,000 grams (2)
Premature infants may be considered macrosomic if their weight exceeds the 90th percentile for gestational age, although some researchers have suggested a more stringent approach (95th percentile or even 97.75th percentile) (1).
How common is fetal macrosomia?
In the United States, approximately 8 percent of term babies have macrosomia grade 1, and 1.1 percent have macrosomia grade 2. The prevalence of macrosomia varies greatly by country (1).
Causes of fetal macrosomia
Maternal and fetal hyperglycemia (high blood sugar) is thought to be a major cause of fetal macrosomia. The baby responds to this excess sugar by releasing insulin, insulin-like growth factors, and growth hormones, which increases fat deposition and fetal size.
Macrosomia often occurs when the mother is obese or has diabetes, particularly gestational diabetes (1). In some instances, macrosomia can also be caused by fetal medical conditions or genetic factors (3).
Risk factors for fetal macrosomia
There are many factors that increase the risk of macrosomia. When any of these risks are present, the physician should closely monitor the mother and baby for macrosomia and its potential complications. Risk factors for macrosomia include the following:
- Maternal diabetes: Both gestational and pre-gestational diabetes can cause the baby to grow very large.
- Maternal obesity: If a mother is obese or gains excessive weight during pregnancy, macrosomia is more likely.
- Prior delivery of a macrosomic baby: In one study, infants with grade 2 macrosomia were seven times more likely to have a subsequent macrosomic sibling (4).
- Multiparity: Women who have previously given birth (i.e. are “multiparous”) are at higher risk for having a baby with fetal macrosomia. Grand multiparas may be at especially high risk (5).
- Post-term pregnancy: Pregnancies that go beyond 40 weeks have an increased incidence of macrosomia (1).
- Advanced maternal age: Women older than 35 years are more likely to have a baby diagnosed with macrosomia (3).
- A male baby: Male fetuses and infants tend to weigh more than females (1). Most babies who weigh more than 4,500 grams are male (6).
- Ethnic background: African American and Hispanic babies are at higher risk for macrosomia (1).
- Genetic factors: Taller, heavier parents may be more likely to have larger babies (6). Genetic abnormalities such as Pallister-Killian syndrome and Beckwith-Wiedemann syndrome also increase the risk of macrosomia (1).
- Congenital anomalies: Certain congenital anomalies, such as ventricular septal defects and atrial septal defects, are associated with macrosomia (7).
Diagnostic procedures and signs of fetal macrosomia
Macrosomia should be suspected if major risk factors (such as maternal obesity or diabetes) are present. In addition to asking about your medical history, doctors can assess the baby’s size using the following methods (1, 3):
- Ultrasound: Ultrasound technology is the most accurate method used to estimate fetal size. Hadlock’s formula (which takes into account head circumference, abdominal circumference, and femur length) is thought to be the most accurate sonographic method for estimating fetal weight.
- Fundal height measurement: The fundal height refers to the length from a woman’s pubic bone to the top of her uterus. A higher than normal fundal height could indicate macrosomia.
- Palpation of the maternal abdomen: Physicians can estimate fetal weight by palpating the mother’s abdomen (a common method is called the “Leopold maneuver”).
- Checking amniotic fluid level: An excess of amniotic fluid (polyhydramnios) can be indicative of macrosomia because larger babies produce more urine (late in pregnancy, the amniotic fluid is made up primarily of fetal urine).
- Nonstress test: This records the baby’s heart rate when they move. Abnormal results of a nonstress test should be taken as a warning sign that something may be wrong with the pregnancy or the baby.
- A biophysical profile (BPP): This uses the nonstress test in conjunction with ultrasound to check the baby’s movements, heart rate, and level of amniotic fluid.
If macrosomia is suspected, physicians should recommend frequent prenatal testing in order to assess fetal well being and determine whether medical intervention is necessary.
Preventing and managing fetal macrosomia
Doctors should advise obese and diabetic women to take certain precautions before attempting to become pregnant, in order to avoid fetal macrosomia and other complications. Pre-pregnancy weight loss can reduce the risk of macrosomia in obese women, and is a very important intervention because it is generally not safe to lose a substantial amount of weight during pregnancy. Management of diabetes before and during pregnancy can also reduce the likelihood of macrosomia (1). General practitioners should refer obese and diabetic women to maternal-fetal specialists who can help them achieve health goals.
If the physician suspects macrosomia, a vaginal delivery still may be occasionally attempted, but only with the informed consent of the mother. More typically, cesarean section is recommended for suspected macrosomia. There are a variety of risks associated with vaginal delivery of a macrosomic baby, including shoulder dystocia (a complication in which the baby’s shoulder gets stuck behind the mother’s pelvic bone), birth trauma, and HIE. Use of Instruments such as forceps and vacuum extractors is associated with a 50% chance of shoulder dystocia in deliveries involving macrosomia (and in general, these instruments increase the risk of shoulder dystocia) (6). If doctors apply excessive force to deliver a baby with shoulder dystocia, this can lead to brachial plexus injury and other forms of damage. Thus, risk factors for shoulder dystocia should be carefully reviewed prior to utilization of forceps and vacuum extractors. Physicians should try and avoid the procedure if substantial risk appears to be present.
If the pregnancy is allowed to run its course, or if induction is attempted, the physician should be prepared to deliver by C-section in the event of an emergency. In addition to shoulder dystocia, deliveries involving macrosomia are at higher risk for prolonged/arrested labor and birth asphyxia (3), among other issues (see next section).
Early/near-term induction of labor with drugs such as Pitocin (synthetic oxytocin) could theoretically reduce complications associated with macrosomia (since the baby will be slightly smaller when delivered), but some studies have found that labor induction does not reduce the risk of complications associated with macrosomia, and might increase the need for a C-section (8). More recent studies have found some purported benefits, but the American College of Obstetrics and Gynecologists (ACOG) still recommends against induction of labor in cases involving large for gestational age babies.
According to ACOG, If the mother has diabetes and the baby likely weighs more than 4,500 grams, a C-section may be the safest method of delivery. A C-section will also likely be recommended if the baby weighs 5,000 grams or more, even if the mother does not have diabetes (6).
After delivery, the baby will likely be examined for signs of birth injuries, abnormally low blood sugar (hypoglycemia), and a blood disorder that affects the red blood cell count (polycythemia) (9).
Fetal complications and birth injuries associated with macrosomia
The following are just a few examples of complications and birth injuries that a macrosomic baby may experience.
- Injuries from forceps and vacuum extractors: Excessive force from inappropriate use of these instruments can cause trauma and conditions such as brachial plexus injuries, intracranial hemorrhages (brain bleeds), seizures, and cerebral palsy.
- C-section: Macrosomia increases the likelihood that a C-section (planned or emergent) will be necessary. If a baby becomes lodged in the birth canal, it is very important to get them out quickly. Delaying a C-section can result in permanent brain damage. The medical team must be well prepared for this possibility.
- Hypoxic-ischemic encephalopathy (HIE): This is a type of brain injury in which a baby is severely deprived of oxygen, resulting in cell death and, often, permanent conditions such as cerebral palsy, seizures, and learning disabilities. This happens many times when the baby is too big to fit through the birth canal and gets stuck or if the umbilical cord becomes compressed.
- Uterine rupture: If a mother had a prior C-section or major uterine surgery, macrosomia increases the risk of uterine rupture (3), a serious complication in which the uterus tears open along the surgical scar line. Indeed, prior uterine surgery can increase the risk of uterine rupture even in the absence of macrosomia. Uterine rupture can cause serious problems such as HIE, and puts the lives of both the mother and baby in danger.
Macrosomia, birth injuries, and medical malpractice
When risk factors for macrosomia are present, it is essential that the physicians monitor the mother and baby very closely and be prepared for a potential delivery by C-section. In certain situations, it may be necessary to plan to deliver the baby early. There are many issues physicians must examine when facing macrosomia. It is crucial that the physician and the medical team be very skilled in handling all issues pertaining to the pregnancy and delivery. It is negligence when a mother and baby are not properly assessed and monitored. Failure to act skillfully and, if necessary, quickly, also constitutes negligence. If this negligence leads to injury of the mother or baby, it is medical malpractice.
Listed below are issues that may constitute negligence:
- Obstetrical instruments (forceps or vacuum extractors) were inappropriately placed or misused.
- There was a failure to order a necessary C-section.
- The physician caused a birth injury by forcing a vaginal birth.
- A physician failed to act promptly during an emergency.
- Pitocin/oxytocin was used improperly.
- The physician failed to give the patient adequate information on the risks and alternatives of a certain course of action, and/or did not get informed consent.


Birth trauma attorneys handling macrosomia cases since 1997
At ABC Law Centers: Birth Injury Lawyers, we focus solely on birth injury cases. We understand the complex legal issues involved with macrosomia and will help you to obtain the compensation to which you are entitled. While we’re based in Michigan, we help clients all over the country.
Our staff is available to answer your questions, respond to your concerns, and explain your legal options. We do not charge any fee for your consultation or your case unless we win.
Featured Videos
Posterior Position
Hypoxic-Ischemic Encephalopathy (HIE)

Featured Testimonial
What Our
Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on. ABC Law Centers: Birth Injury Lawyers was just that.
- Michael


