Obesity During Pregnancy & Birth Injuries
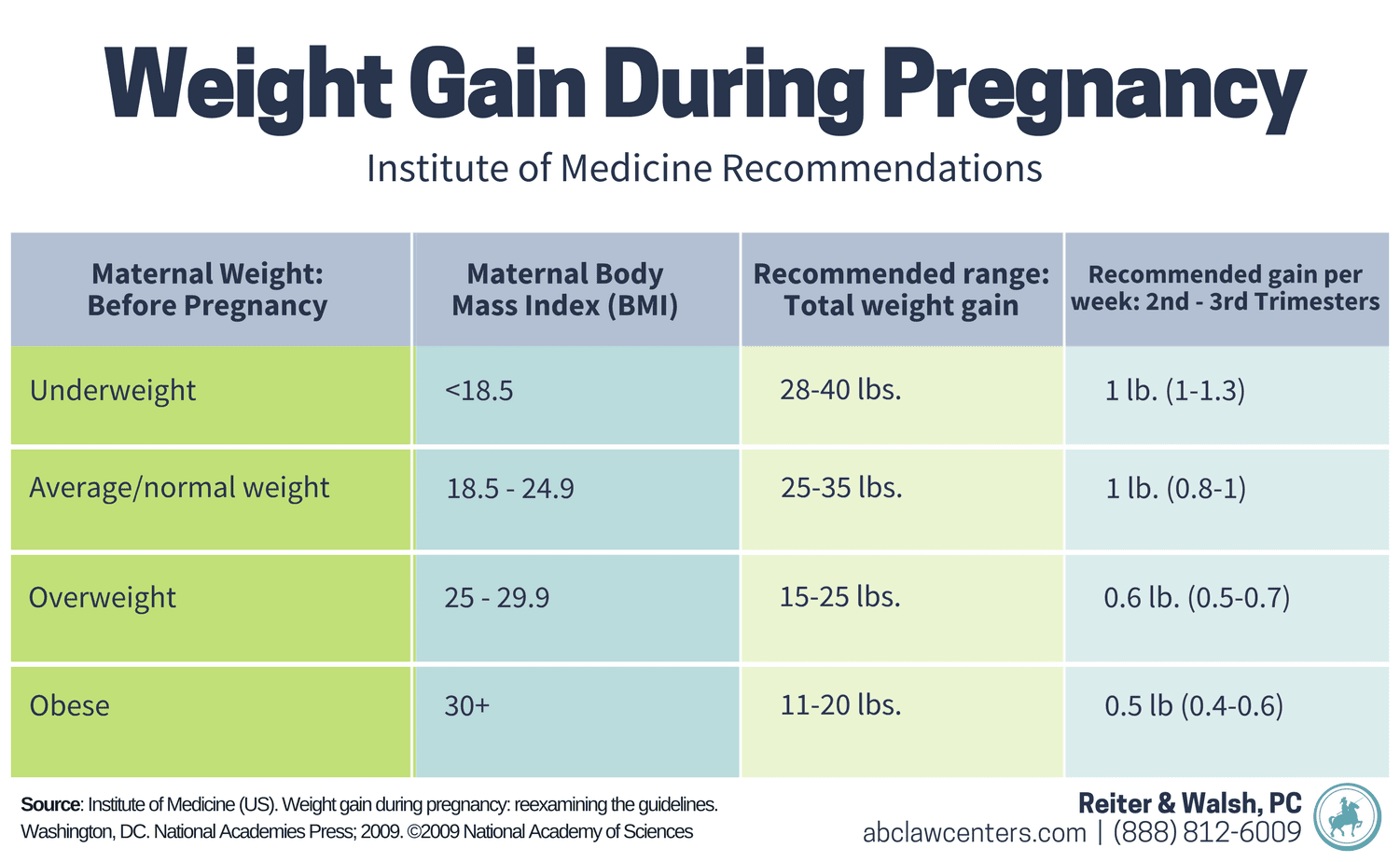
Obesity during pregnancy, or maternal obesity, is defined as a body mass index (BMI) of 30 or more ( ≥ 30 kg/m2) (1). BMI measurements are based on a mother’s weight relative to her height. Excessive weight gain during pregnancy is typically defined as gaining more than 1.5 pounds per week, and exceeding this rate may impact the pregnancy. Maternal obesity can increase the risk of complications during pregnancy and labor/delivery. Because of this, mothers who are obese or gain excessive weight during pregnancy are considered high-risk and should be closely monitored.
Maternal obesity and pregnancy complications
Maternal obesity can increase the risk of several pregnancy complications that can be harmful to the mother and the baby. Below are several pregnancy complications associated with maternal obesity.
Gestational diabetes
Gestational diabetes is a condition in which a mother is diagnosed with diabetes for the first time partway through the pregnancy. Mothers who are overweight are more likely to have pre-existing diabetes, and also more likely to develop gestational diabetes. The more obese a mother is, the greater her potential risk is for developing diabetes. Medical professionals are required to screen mothers for pre-existing diabetes and gestational diabetes during prenatal care appointments (1). This is done using the glucose challenge test. Diabetes during pregnancy may lead to premature birth, macrosomia, neonatal hypoglycemia, and other dangerous complications (2).
Macrosomia
Obese mothers are more likely to carry fetuses that become larger than average and are therefore considered macrosomic. A fetus is generally deemed macrosomic when it weighs more than 4000 grams (1). Macrosomia often develops when a baby has high blood sugar, which is more common when their mothers are obese and/or have diabetes. Macrosomia can cause harmful complications including shoulder dystocia, uterine rupture, prolonged labor, cephalopelvic disproportion (CPD), and increased use of mechanical instruments like forceps or vacuum extractors (3).
Neonatal hypoglycemia
Maternal obesity, especially in the presence of gestational diabetes, can also lead to a condition known as neonatal hypoglycemia. While babies are in utero, they become accustomed to a certain level of blood sugar from their mother and produce a correspondingly high level of insulin to help them metabolize this sugar. When babies are born, they no longer have the high blood sugar supply from the mother, but may still produce a high level of insulin. When this happens, the baby’s blood sugar can drop dangerously low, resulting in neonatal hypoglycemia. This condition puts the baby’s brain at risk because brain cells use glucose as an energy source. Without glucose, cells can begin to die. Babies whose mothers are obese and/or have diabetes may need much closer monitoring and more frequent feeding postnatally to prevent dangerous blood sugar crashes (4).
Intrauterine growth restriction (IUGR)
Contrary to intuition, in some cases obesity during pregnancy can cause intrauterine growth restriction (IUGR), a condition in which the fetus grows slower than expected. While in utero, babies of obese mothers may experience hormonal and physical changes that can lead to low birth weight (5). Babies with IUGR are often more fragile, less developed, and more susceptible to oxygen deprivation, especially during contractions or labor and delivery. Due to these factors, small babies may not be able to tolerate the process of labor and are often most safely delivered via c-section before term.
High blood pressure/preeclampsia
Mothers who are obese may have an increased risk of high blood pressure (hypertension) and preeclampsia (high blood pressure that starts during pregnancy) (1). The volume of blood that passes between mother and baby through the placenta is dependent on many factors, one of which is blood pressure. If the mom’s blood pressure is too high, resistance increases and blood flow to the baby decreases in a condition called reduced uteroplacental perfusion (RUPP). Because the placenta supplies oxygen and other nutrients, hypertension can mean reduced supplies of both to the baby. High blood pressure and preeclampsia must be carefully managed and monitored to avoid birth injury and other complications including placental abruption, premature birth, IUGR, and more. For further information about managing maternal high blood pressure and preeclampsia, click here.
Maternal obesity and labor and delivery complications
Vaginal birth after c-section (VBAC)
Obese mothers who have previously had a c-section are less likely to have a successful vaginal birth after c-section (VBAC) than are their counterparts with normal BMIs (1). In a large prospective multicenter study, the rate of failed trials of labor after c-section (TOLAC) increased from 15 percent in normal-weight mothers to 30 percent in obese mothers, and to 39 percent in severely obese mothers. In addition, the rate of uterine rupture increased with maternal weight (6). Physicians must thoroughly explain all these risks to their patients. In addition, every delivery unit should have the capability to perform a prompt emergency c-section if necessary, especially for obese mothers attempting a VBAC.
Fetal monitoring errors
Fetal heart rate monitoring is a critical component of assessing a baby’s health in utero. While a mother is in labor, physicians should be assessing the baby’s well-being with a fetal heart rate monitor. In many cases, doctors use external monitors, but it’s important to note that individuals who are overweight or obese may have accumulations of soft tissue that can make external monitoring more difficult (1). It is important to ensure that the monitor is accurately picking up the fetal heart rate tracings to know if the baby is tolerating labor well. If possible, an internal fetal monitor should be used for monitoring the baby when mothers are obese to avoid monitoring errors (1).
Prolonged labor and increased use of labor drugs
Labor traditionally progresses in a certain approximate pattern, but this pattern can be altered by numerous factors, including a mother’s weight. Mothers with a high BMI tend to have a longer first stage of labor, which is associated with an increased risk of prolonged or arrested labor (1). Prolonged or arrested labor can lead to serious complications for both the mother and the fetus (read more here).
In order to avoid the risks associated with prolonged and arrested labor, physicians may consider using labor drugs (such as Pitocin and Cytotec) to speed up the delivery, which can be very dangerous. These drugs make labor contractions stronger, longer, and with too little rest in between contractions, but the effects of these drugs are unpredictable: the same dose in one mother may have only a small effect, while in another it may cause uterine hyperstimulation, making contractions too frequent, long, and/or intense. To learn more about the dangers of labor drugs, check out this page. In addition to these risks, obese women are less likely to have a successful labor induction (1), meaning that these drugs often fail to produce the desired result. In cases of prolonged and arrested labor, a c-section should always be considered.
Anesthesia complications
Compared to mothers within the normal weight range, obese mothers have a higher rate of the following (1):
- Failed labor anesthesia and analgesia
- Difficult breathing tube placement (intubation)
- Low blood pressure (hypotension)
- Fetal heart rate decelerations (nonreassuring heart tracings)
These complications can delay the administration of a necessary c-section, which can have severe consequences for the mother and child. Obese mothers should be evaluated by an anesthesiologist before or early in labor so the medical team is more prepared for intubation, anesthesia administration, and other procedures related to C-section.
Maternal obesity and birth injuries
Obesity increases the risk of numerous health complications such as diabetes and hypertension (high blood pressure) in everyone, not just pregnant women. In pregnancy, obesity and its associated conditions can pose a risk to the baby, necessitating closer monitoring during pregnancy and labor and more frequent follow-up after testing. If maternal obesity is not managed properly, it can lead to the pregnancy, labor, and delivery complications detailed above. If these complications are not treated correctly, serious birth injuries and infections may result. Issues commonly associated with maternal obesity include (1, 7):
- Hypoxic-ischemic encephalopathy (HIE)
- Cerebral palsy
- Neonatal sepsis
- Respiratory distress syndrome
- Epilepsy/seizure disorder
- Neonatal hypoglycemia
If pregnancy complications associated with maternal obesity are mismanaged, this is medical negligence. If this negligence leads to birth injury or disability in the baby, this is medical malpractice.
Maternal obesity: ensuring a healthy pregnancy and delivery
Obesity is a major risk factor for birth injury, and it’s critical that medical professionals treat it as such. Mothers and their babies must receive care that addresses their unique needs throughout pregnancy, labor, and delivery. This includes:
- Proper counseling and evaluation before pregnancy (if possible)
- Proper monitoring throughout pregnancy
- Proper treatment of underlying medical issues
- Continual assessment of the baby’s growth and well-being
One of the critical components of ensuring pregnancy health is antenatal testing. During pregnancy, medical staff should conduct numerous tests to ensure that both the mother and baby are progressing through the pregnancy as expected. Tests included as part of this monitoring should include:
- Non-stress tests (NSTs) to record the baby’s vigor, movement, and heartbeat, using an electronic fetal monitor and fetal ultrasound
- Biophysical profiles (BPPs), which measure the baby’s rate, muscle tone, movement, breathing, and the amount of amniotic fluid around the baby, often in conjunction with an NST
- Amniotic fluid index (AFIs) to see how much amniotic fluid surrounds your baby; these are often provided as part of a BPP
- Doppler flow monitoring to test whether the baby is getting adequate blood flow to the brain, organs, and extremities
In many cases, early scheduled C-section is indicated when a mother’s due date nears or testing shows abnormalities. If an obese or overweight mother is attempting vaginal delivery, the delivery unit must have the capacity to perform an emergency C-section if it becomes necessary.


Call the trusted birth injury attorneys at ABC Law Centers: Birth Injury Lawyers
The birth injury attorneys at ABC Law Centers: Birth Injury Lawyers solely handle birth injury cases, and can help if you or your child were injured as a result of poor care during pregnancy, labor, or delivery. Medical professionals must meet the ‘standards of care’ – if your doctor did not provide proper care for you and your child, feel free to call us for a free consultation. Our birth injury attorneys are compassionate, driven, and already ready to speak with you. Your information is always 100 percent confidential, and you will pay no legal fees until we win or settle your case.
Featured Videos
Posterior Position
Hypoxic-Ischemic Encephalopathy (HIE)

Featured Testimonial
What Our
Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on. ABC Law Centers: Birth Injury Lawyers was just that.
- Michael
Helpful resources
- Ramsey, P. S., & Schenken, R. S. (2019, May). Obesity in pregnancy: Complications and maternal management. Retrieved from https://www.uptodate.com/contents/obesity-in-pregnancy-complications-and-maternal-management.
- ABC Law Centers: Birth Injury Lawyers. (n.d.). Gestational Diabetes & Birth Injuries. Retrieved from https://www.abclawcenters.com/practice-areas/gestational-diabetes-signs-causes-and-risk-factors//.
- ABC Law Centers: Birth Injury Lawyers. (n.d.). Fetal Macrosomia. Retrieved from https://www.abclawcenters.com/practice-areas/macrosomia//.
- ABC Law Centers: Birth Injury Lawyers. (n.d.). Neonatal Hypoglycemia and Birth Injury. Retrieved from https://www.abclawcenters.com/practice-areas/neonatal-hypoglycemia//.
- Radulescu, L., Munteanu, O., Popa, F., & Cirstoiu, M. (2013, September 15). The implications and consequences of maternal obesity on fetal intrauterine growth restriction. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3806033/.
- Metz, T. D. (2019, April). Choosing the route of delivery after cesarean birth. Retrieved from https://www.uptodate.com/contents/choosing-the-route-of-delivery-after-cesarean-birth.
- Blomberg, M. (2013, July 01). Maternal Obesity, Mode of Delivery, and Neonatal Outcome. Retrieved from https://insights.ovid.com/pubmed?pmid=23743457.


