Signs of Fetal Distress During Pregnancy and Delivery
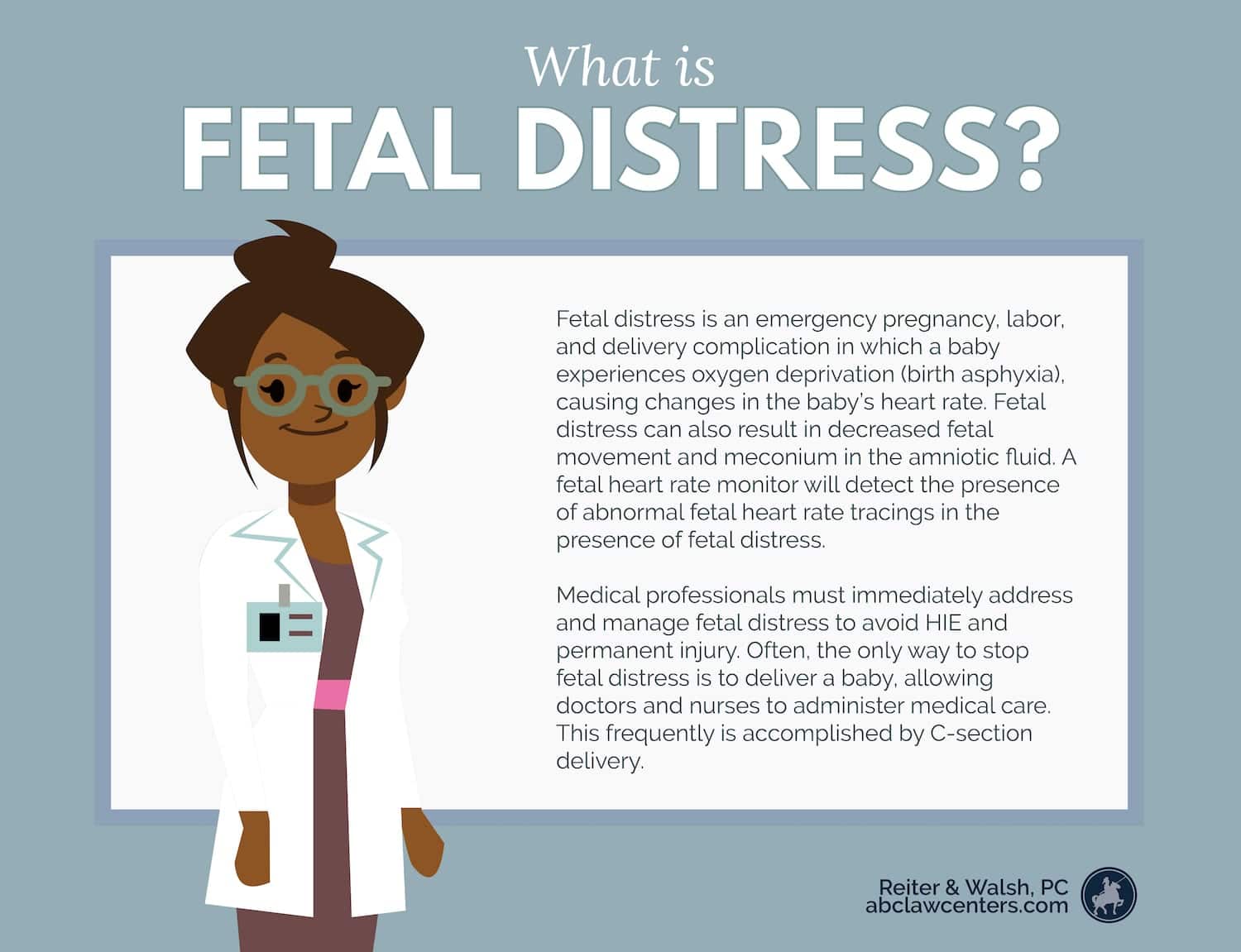
Fetal distress is an emergency pregnancy, labor, and delivery complication in which a baby may experience oxygen deprivation (birth asphyxia).
Fetal distress is also called fetal intolerance to labor.
Signs of fetal distress may include:
- Abnormal changes in the baby’s heart rate (as seen on a fetal heart rate monitor)
- Decreased fetal movement
- Meconium in the amniotic fluid (increasing risk for meconium aspiration)
Medical staff should monitor for these signs, among others. They must immediately address and manage fetal distress to avoid serious complications, such as hypoxic-ischemic encephalopathy (HIE), and other birth injuries. Long term consequences can include conditions like cerebral palsy (CP).
Often, the only way to stop fetal distress is to deliver a baby. Doctors and nurses can then administer medical care. Medical staff usually deliver the baby by emergency C-section delivery.
Expectant mothers aren’t always with their physician when signs of fetal distress occur. The following signs may indicate a baby is in trouble.
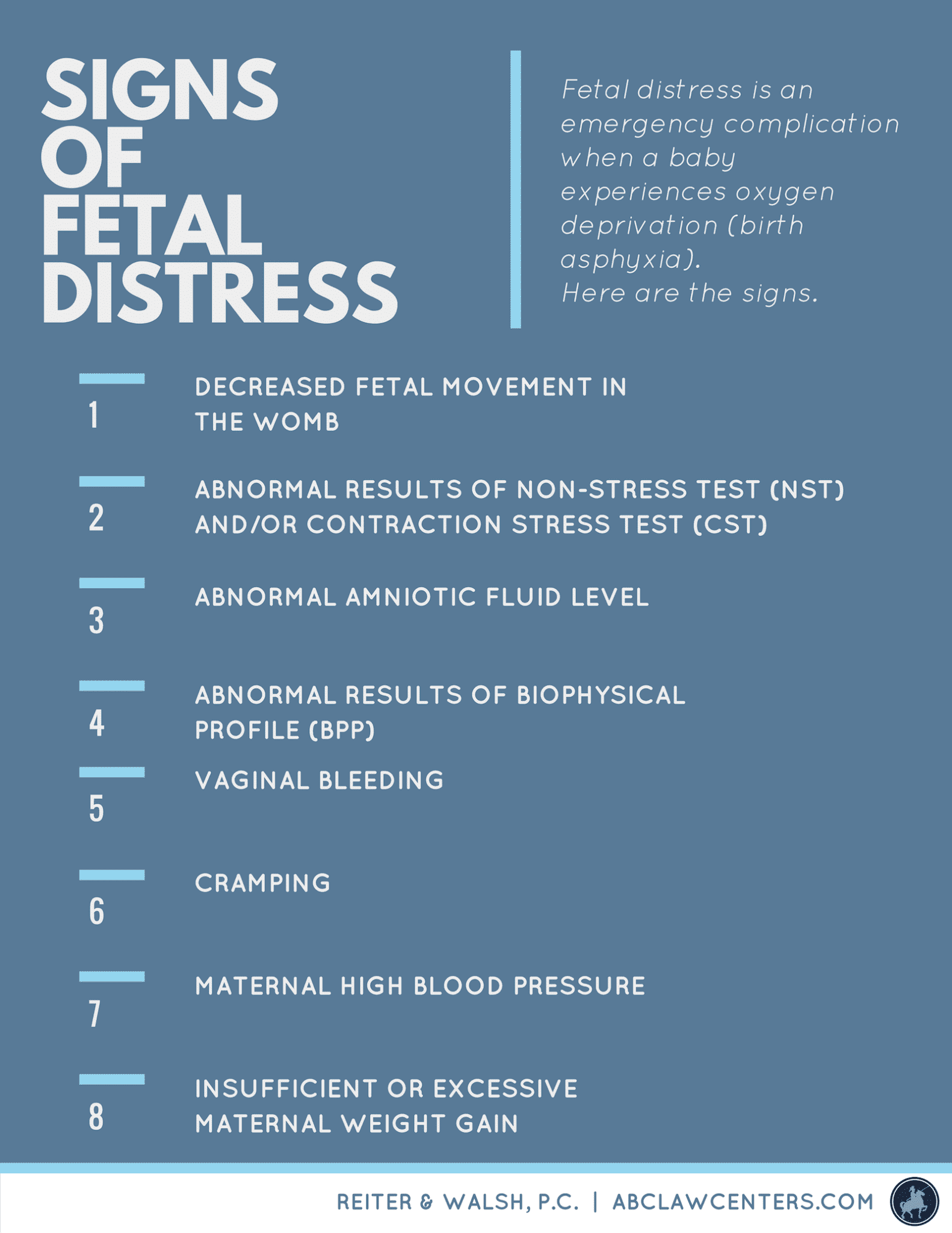
8 Common Signs of Fetal Distress
Decreased Fetal Movement in the Womb
Beyond bringing joy to the family, movement within the womb is an important indicator of the baby’s health. Regular pauses in movement are normal, such as when babies sleep in the womb. However, if the baby becomes less active or completely ceases movement, this may be a cause for concern. Physicians should ask expectant mothers about fetal movement and conduct additional testing if patterns are abnormal.
Abnormal Fetal Heart Rate
Some fetal heart rate patterns indicate distress. Medical professionals observe an unborn baby’s heart rate with either an external or internal fetal monitoring device. External monitoring uses a belt-like device strapped around a mother’s abdomen. Internal monitoring involves attaching an electrode to the baby’s scalp.
In a healthy labor and delivery, the baby’s heart rate will have variability, with accelerations indicating fetal movement. The normal range for the baby’s heart rate is between 110-160 beats per minute.
The following fetal heart rate patterns are examples of nonreassuring patterns that warrant further investigation and/or medical intervention:
- An abnormally fast heart rate (tachycardia)
- An abnormally slow heart rate (bradycardia)
- Abrupt decreases in heart rate (variable decelerations)
- Late returns to the baseline heart rate after a contraction (late decelerations)
- Decreased heart rate variability
- Lack of fetal heart rate accelerations
An abnormal fetal heart rate can appear on prenatal testing including a non-stress test (NST) or a contraction stress test (CST).
Tell us your story.
Dealing with a birth injury diagnosis can be difficult, but our attorneys can help. The ABC Law Centers: Birth Injury Lawyers team focuses exclusively on birth injury and are dedicated to earning justice for families like yours.
How does a non-stress test (NST) work?
During an NST, a medical professional looks at how the baby’s heart rate changes when the fetus moves. A normal NST is called “reactive,” meaning that the baby’s heart rate went up and down as expected. “Non-reactive” means that the baby’s heart rate did not increase enough at times during the test. Physicians may also classify NST results into these categories:
- Normal
- Requiring further testing and possibly delivery
- An emergency C-section is necessary
How does a contraction stress test (CST) work?
A CST helps predict how the baby will cope during the labor process. This test determines whether it is safe to proceed with a vaginal delivery. Uterine contractions temporarily restrict oxygen flow. A healthy baby can tolerate this temporary restriction, but it may be very dangerous for a baby in distress. During a CST, physicians record the baby’s heart rate in response to contractions.
If conducting a CST on a woman not yet in labor, the physician may give her Pitocin (synthetic oxytocin), to make the uterus contract. There are certain risks associated with this medication. Pitocin can cause uterine tachysystole, or contractions that are too strong, too frequent, or too long. Uterine tachysystole can severely restrict oxygen flow to the baby and sometimes leads to uterine rupture, placental abruption, or HIE.
Abnormal Amniotic Fluid Level
The amount of amniotic fluid can also be an indication of fetal distress. Abnormally low amniotic fluid (oligohydramnios) can lead to oxygen deprivation and birth injuries like HIE and cerebral palsy (CP).
A trending decrease in amniotic fluid may also warn of oligohydramnios. Medical staff should watch closely for this condition.
Abnormally high amniotic fluid volume is called polyhydramnios. Polyhydramnios can also cause oxygen deprivation and subsequent birth injuries.
Abnormal Results of Biophysical Profile (BPP)
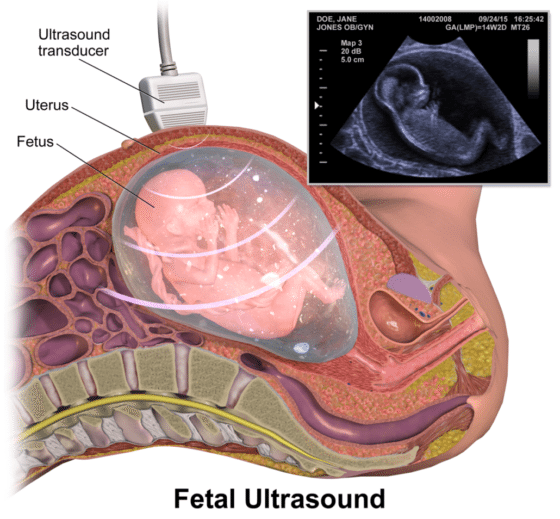
If the results of an NST are non-reactive or nonreassuring, medical staff can perform a biophysical profile (BPP). The BPP includes both the NST results and an ultrasound. The profile assesses fetal movement, breathing, tone, and amniotic fluid volume.
The BPP scores five parameters, including the nonstress test and four ultrasound parameters. Each category scores either zero or two points. A score of four or lower indicates fetal distress and requires immediate action. A total score of eight or higher is normal.
If the ultrasound finds low amniotic fluid, medical staff should take action. Low amniotic fluid can put the baby at risk for umbilical cord compression. In that circumstance, admission to the hospital, close fetal monitoring, and delivery are required. Otherwise, the cord compression puts the baby at risk of not getting enough oxygen.
Vaginal Bleeding
Small amounts of vaginal bleeding are fairly common during pregnancy. However, bleeding can also be an indication that something is wrong with the pregnancy.
One particularly dangerous example is placental abruption, when the placenta tears away from the uterus. Placental abruption deprives the baby of oxygen. Depending on the location and size of the abruption, it may not initially cause fetal distress. However, the health of both mother and baby could still be in jeopardy, especially if the tear grows.
A placental abruption can be present with no vaginal bleeding. (Bleeding can be retained behind the placenta.) Placental abruption is always a serious risk.
A placental abruption and any other placental abnormalities that cause bleeding require very close monitoring. In many cases, the mother should be admitted to the hospital and given an emergency C-section.
Cramping
Some cramping is relatively normal during pregnancy. As the baby grows, the uterus needs to expand, which can cause cramping. In some cases, cramping may indicate something more serious, such as:
- miscarriage
- placental abruption
- preeclampsia
- a urinary tract infection
- preterm labor
Physicians need to listen to patients who experience cramping. They should perform proper tests to ensure the health of the mother and baby.
Maternal High Blood Pressure
If a mother has high blood pressure during pregnancy, it can cause symptoms like:
- low birth weight
- preeclampsia
- placental abruption
- stroke
- preterm birth
- hypoxic-ischemic encephalopathy (HIE)
High blood pressure during pregnancy requires early delivery, typically by 37 weeks gestation.
Tell us your story.
Dealing with a birth injury diagnosis can be difficult, but our attorneys can help. The ABC Law Centers: Birth Injury Lawyers team focuses exclusively on birth injury and are dedicated to earning justice for families like yours.
Insufficient or Excessive Maternal Weight Gain
Experts believe that a weight gain of anywhere between 25 and 35 pounds is normal during pregnancy. However, the ranges can vary. Doctors may recommend different weight changes for women who were under or overweight before becoming pregnant. Mothers carrying twins or multiples may also require different recommendations.
What does it mean if my baby is extremely small?
If a mother doesn’t gain enough weight, the fetus may be in distress. The baby may have a condition called intrauterine growth restriction (IUGR). IUGR is when the baby is smaller than is developmentally appropriate, which can relate to other problems.
IUGR requires careful physician monitoring and testing, and often early delivery prior to labor. IUGR babies typically do not tolerate contractions during labor and may not get enough oxygen. A mother should have regular prenatal visits. Her physician should know that abnormal weight changes may necessitate additional fetal monitoring.
What if my baby is too large?
Excessive maternal weight gain may lead to giving birth to an abnormally large baby. This circumstance is called macrosomia. Macrosomia can create a risky birth situation, especially dangerous if the physician is unaware of the condition. It can cause labor issues such as:
- Cephalopelvic disproportion (CPD), where the mother’s pelvis is too small to accommodate the size of the baby’s head
- Shoulder dystocia, in which the baby’s shoulder gets stuck on the mother’s pelvic bone during delivery
- Hypoxic-ischemic encephalopathy (HIE)
Often, the best way to deliver a macrosomic baby is by C-section.
A Note On Terminology
The American College of Obstetricians and Gynecologists (ACOG) cautions that the term fetal distress is “imprecise and nonspecific.” Instead, they recommend replacing “fetal distress” with “nonreassuring fetal status.” Medical professionals should further categorize a baby’s status into three separate groups to better describe the situation.
Regardless of terminology, medical professionals must be very familiar with specific warning signs of fetal oxygen deprivation to prevent permanent harm.
Tell us your story.
Dealing with a birth injury diagnosis can be difficult, but our attorneys can help. The ABC Law Centers: Birth Injury Lawyers team focuses exclusively on birth injury and are dedicated to earning justice for families like yours.
What causes fetal distress?
The following are just a few underlying causes of fetal distress:
- Abnormal fetal presentation
- Forceps and vacuum extractor misuse
- Placental abruption
- Preeclampsia
- Prolonged and arrested labor
- Umbilical cord problems
- Uterine rupture
How is fetal distress treated?
The medical team must skillfully and continuously monitor fetal well-being throughout pregnancy, labor, and delivery. They are responsible for recognizing and responding to signs of fetal distress.
If a baby is in distress,
appropriate interventions to get more oxygen to the baby may include:
- Oxygen for the mother
- Fluids or medication for the mother
- Change in the mother’s position
Often, an emergency C-section is required to remove the baby from the conditions causing the fetal distress. A C-section should occur especially if earlier interventions did not cause fetal heart tones to become reassuring.
An emergency C-section delivery should occur within 3 to 18 minutes, depending on the circumstances, and sometimes sooner.
Nonreassuring Fetal Heart Tracings
An electronic fetal monitor records the mother’s contractions and the baby’s heart beat in response to the mother’s contractions. When a fetal heart tracing is nonreassuring, it means that the baby is in distress and is not getting enough oxygen. Prompt and appropriate actions must be taken when this occurs.
The normal baseline fetal heart rate is 110 – 160 beats per minute (bpm). A deceleration is a decrease in the fetal heart rate below the baby’s baseline heart rate. Values below 110 bpm are termed bradycardia (slow heart rate). An abrupt descent of the fetal heart rate can be caused by cord compression. In general, decelerations are caused by a sudden reduction in oxygen or a stepwise decrease in oxygen to the baby caused by maternal low blood pressure or hypertonic contractions (contractions that are so fast and strong that they can deprive the baby of oxygen – this can occur when Pitocin or Cytotec are given).
Bradycardia is very serious and can be caused by hypoxia, or it may be the cause of hypoxia. Bradycardias that occur near the end of the second stage of labor can lead to hypoxia if sufficiently prolonged and severe. These bradycardias can be the result of head compression and sudden umbilical cord compression. If bradycardia becomes severe, oxygen and carbon dioxide transfer will become impaired and the baby’s blood will become acidic, which is what occured in this case.
Indeed, when the fetal heart rate is under 100 bpm for more than 3 – 5 minutes – independent of uterine contractions – it means the baby is not getting enough oxygen and severe asphyxia is occurring. This is an emergency and means the baby must be delivered immediately by C-section to avoid or decrease brain damage.
Mismanaged fetal distress can lead to birth injury
Signs of fetal distress should always be taken seriously. Medical professionals must promptly recognize and address these signs to prevent permanent injury and disability in a newborn baby.
They must be especially careful in assessing maternal and fetal health in high-risk pregnancies. Physicians must follow standards of care for high-risk pregnancies. If physicians dismiss signs of fetal distress, this is medical negligence. If this negligence leads to injury, it is medical malpractice.
Should I contact a birth injury attorney?
If medical staff ignore fetal distress, the baby can suffer permanent consequences. It can be frustrating to learn that medical negligence caused an injury to your baby. However, consulting with an attorney can help you understand your legal options.
Birth injury is a challenging area of law to pursue due to its complex nature. At ABC Law Centers, our attorneys focus exclusively on this type of medical malpractice law. We pursue cases that have to do with birth injury, hypoxic-ischemic encephalopathy (HIE), and cerebral palsy.
To find out if you have a case, contact our firm to speak with one of our attorneys. A consultation is completely free, and you will pay no fees unless we win your case. We give personal attention to each child and family we help, and are available 24/7 to speak with you.
★★★★★
“My experience with Jesse Reiter and his staff was amazing. I had been to two different law firms regarding my son and was told there was no case. I heard about Jesse and his firm from a newspaper article and thought I would give it another shot. Within 30 minutes of talking with Jesse while he was going over my sons hospital reports, he told me there was definitely a case. Jesse and his staff never made me wonder what was ‘happening with the case.’ They always filled me in on everything. I felt included. Any questions that I had were answered very quickly. Jesse and his team became to be like an extended family to us. I will forever be grateful for the hard work, dedication and the fight they fought for my son.”
-Client review from 10/16/2016
Tell us your story.
Dealing with a birth injury diagnosis can be difficult, but our attorneys can help. The ABC Law Centers: Birth Injury Lawyers team focuses exclusively on birth injury and are dedicated to earning justice for families like yours.
Disclaimer: Please know that our website is owned by a birth injury law firm that focuses exclusively on birth injury cases. We try to provide useful medical information to our readers, but we cannot provide treatments or medical advice or treatments. If you might be having a medical emergency, please call 911 and seek immediate medical attention.
Sources
- Hofmeyr, G. J., & Novikova, N. (2012). Management of reported decreased fetal movements for improving pregnancy outcomes. The Cochrane database of systematic reviews, 4, CD009148.
- Fetal Heart Monitoring: What’s Normal, What’s Not?
- Fetal Distress: Diagnosis, Conditions & Treatment
- Monitoring your baby before labor: MedlinePlus Medical Encyclopedia
- Assessment of amniotic fluid volume
- Biophysical profile test for antepartum fetal assessment
- Placental abruption: Pathophysiology, clinical features, diagnosis, and consequences
- Cramping During Pregnancy: Causes, Treatment & Prevention
- Weight Gain During Pregnancy | Maternal Infant Health | CDC
- Fetal Growth Restriction– Stanford Children’s Health
- Fetal Macrosomia
- Committee on Obstetric Practice. (2005). ACOG Committee Opinion. Number 326, December 2005. Inappropriate use of the terms fetal distress and birth asphyxia. Obstetrics and gynecology, 106(6), 1469.
- Intrapartum category I, II, and III fetal heart rate tracings: Management