We have written extensively about the importance of quickly delivering a distressed baby in order to prevent brain damage caused by a lack of oxygen in the baby’s brain. A delayed emergency C-section delivery can occur for a number of reasons, including giving birth at home. A recent case in which an unlicensed midwife could not quickly deliver a baby when the mother’s uterus (womb) ruptured and the baby had a prolapsed umbilical cord is a sad reminder of the critical importance of an emergency C-section delivery.
A mother in Alabama had an uneventful pregnancy and wanted to give birth at home, so she sought the help of a midwife. During the home delivery, the mother’s uterus ruptured and the baby’s umbilical cord fell in front of her in the birth canal, which is called an umbilical cord prolapse. Both conditions can cause severe oxygen deprivation in the baby and require immediate delivery. Since the birth was not at a hospital, an ambulance had to be called to rush the mother and her oxygen-deprived baby to the hospital. Sadly, too much valuable time was wasted. The baby’s brain was starved of oxygen for too long, causing her to have severe brain damage.
The midwife was charged with practicing nurse midwifery without a license and was sentenced to probation and ordered to stop delivering babies in Alabama.
WHAT IS UTERINE RUPTURE & WHAT ARE THE CAUSES?
A ruptured uterus is a tear through all layers of the uterine wall. This is an obstetrical emergency because it can cause severe hemorrhaging in the mother, which can cause oxygen deprivation (birth asphyxia) in the baby. A ruptured uterus can cause birth asphyxia in multiple ways:
- The rupture causes the mother to lose so much blood that she is unable to deliver adequate oxygen-rich blood to the baby. The mother may even have such a loss of blood volume that she goes into shock, which is life-threatening for the mother and baby.
- The tear is at or very close to the placenta and it severs vessels involved in uteroplacental circulation, thereby reducing the amount of blood going to the baby.
- The rupture affects the placenta. One study found that 18% of uterine ruptures occurred when placental abruption was present and the uterus was unscarred.
- If the baby moves into the mother’s abdomen when the uterus is ruptured, many serious medical complications can occur, such as the umbilical cord becoming stretched, compressed or torn.
The location and extent of the tear and the baby’s reserves play a role in the severity of the birth asphyxia. Regardless of the extent of the rupture, the baby must be delivered by emergency C-section as soon as a rupture occurs in order to prevent the baby from being severely oxygen deprived.
A ruptured uterus usually occurs when there is scarring from surgeries, such as a previous C-section delivery or uterine or abdominal surgeries. Indeed, a vaginal birth after C-section delivery (VBAC) is the biggest risk factor for uterine rupture.
Listed below are causes of and risk factors for a uterine rupture.
Causes of & Risk Factors for Uterine Rupture
- Vaginal birth after C-section delivery (VBAC)
- A scarred uterus
- Cephalopelvic disproportion (CPD). This occurs when the mother’s pelvis is too small for the size of the baby, resulting in the baby being unable to pass through the birth canal.
- Malpresentation. This is when the baby is not in the normal head-first position. Malpresentations include brow, face, breech and shoulder presentations.
- Grand multiparity. This is when the mother has given birth 5 or more times.
- Use of Pitocin, Cytotec or other labor induction drugs. This is probably the leading cause of rupture of the unscarred uterus. Pitocin can cause contractions to be too strong and too frequent, which puts a lot of strain on the uterus.
- Placental abruption. This is when the placental lining separates from the uterus. This can cause the baby to be either partially or completely cut off from the mother’s circulation.
- Forceps use and internal version. Using a delivery device such as forceps increases the risk of a ruptured uterus, as does performing internal version. Internal version is when the physician inserts a hand into the womb and grasps the baby by one or both feet to turn her.
- Multiple fetuses (twins, triplets, etc.)
- Post-term labor
- Maternal obesity
- Difficult labor
- A large for dates baby (large for gestational age (LGA)
- Previous uterine rupture
- When Pitocin is used in the presence of other risk factors for uterine rupture, such as malpresentation or a previous C-section scar, it is extremely dangerous. In fact, using Pitocin when these conditions are present is contraindicated.
There are many obstetrical emergencies that require prompt C-section delivery. The mother and baby can deteriorate very quickly when uterine rupture occurs which is why it is crucial to have a medical team present that can quickly perform surgical interventions.
WHAT IS UMBILICAL CORD PROLAPSE & WHAT ARE THE CAUSES?
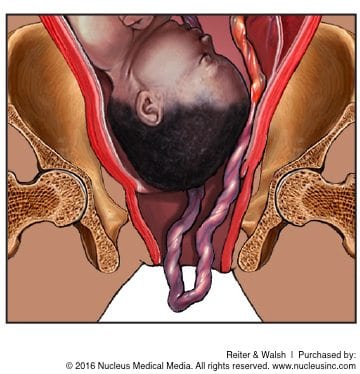 Normally, the umbilical cord exits the birth canal after the baby. An umbilical cord prolapse occurs when the baby’s cord descends through the birth canal before (in front of) the baby. This is an emergent situation because cord prolapse causes compression of the cord between the baby and the uterus, cervix or pelvic inlet.
Normally, the umbilical cord exits the birth canal after the baby. An umbilical cord prolapse occurs when the baby’s cord descends through the birth canal before (in front of) the baby. This is an emergent situation because cord prolapse causes compression of the cord between the baby and the uterus, cervix or pelvic inlet.
When the cord becomes compressed or impinged upon, the baby can be partially or completely cut off from her supply of oxygen. The baby receives all her oxygen from oxygen-rich blood being delivered to her from the mother. This blood travels from the mother to the baby through vessels in the uterus and placenta (uteroplacental circulation). Blood involved in the uteroplacental circulation lastly travels through the umbilical cord vein and into the baby. Anything that hinders blood flow at any point in this path can cause the baby to experience birth asphyxia.
An overt prolapse occurs when the cord descends in front of the baby, usually through the opening of the cervix, and into or beyond the vagina. In this case, the baby’s membranes are invariably ruptured and the cord can be seen or felt. An occult prolapse is when the cord descends alongside, but not in front of, the presenting part of the baby. In this case, the membranes may or may not be ruptured. In both types of cord prolapse, there will be a fetal heart rate deceleration (decrease in baby’s heart rate below the baby’s baseline rate), which typically will be sudden and prolonged. This is a type of non-reassuring heart tracing indicates that the baby is in distress and must be delivered immediately.
In some cases, the physician may try to deliver the baby vaginally, while moving the baby away from the cord in order to relieve compression and pressure on the cord and reduce the risk of birth asphyxia. Frequently, this course of action fails and an emergency C-section must be performed immediately. While preparing for the C-section, the presenting part of the baby is usually pushed back into the pelvis to try and reduce the pressure on the cord. The cord must be elevated until the baby is out. It is recommended that a baby be delivered within minutes of the onset of a non-reassuring heart tracing / decelerations to avoid permanent brain damage from cord prolapse. Most experts recommend delivery in 12 minutes or less, and delivery should not take longer than 20 minutes.
Risk Factors for Umbilical Cord Prolapse
The risk factors for umbilical cord prolapse are related to maternal / fetal factors that lead to inadequate filling of the mother’s pelvis by the baby. In addition, obstetrical interventions that cause membrane rupture can lead to a cord prolapse. Risk factors for a prolapsed cord are listed below.
- Rupture of the membranes. Whether occurring spontaneously or due to the physician intentionally causing a rupture (amniotomy), the forceful gush of fluid that follows a rupture can carry the cord beyond the presenting part of the baby. This most commonly occurs when there is premature rupture of membranes (PROM), an unengaged presenting part of the baby (baby not descended past narrowest part of pelvis), and polyhydramnios (too much amniotic fluid). If the physician ruptures the membranes too early, the baby’s head is too high up in the womb. The fluid loss and unengaged head in the cervix allow the
 umbilical cord to drop in front of the baby, which can cause compression as the baby descends.
umbilical cord to drop in front of the baby, which can cause compression as the baby descends. - Malpresentation. When the baby is not in the head first position, she is at a higher risk of having a cord prolapse. Thus, vertex, transverse lie and breech (especially footling breech) positions are all risk factors for cord prolapse.
- Prematurity. Premature babies have a higher rate of cord prolapse, which is likely due to the smaller size of the baby relative to the amniotic fluid volume, as well as the fact that premature babies have a high frequency of malpresentation.
- Multiple gestation. The risk of cord prolapse in a term twin pregnancy is confined to the second born, who has an increased probability of malpresentation. The first baby can push /pull out the cord of the next baby upon exiting the mother.
- Multiparity. When women have previously given birth, they are more likely to have a rupture of membranes prior to engagement of the presenting part, which makes it more likely for the cord to move in front of the baby.
Given the need for a very quick delivery when cord prolapse or any other obstetrical emergency is present, a delivery should never occur in a facility that does not have the staff or equipment to promptly deliver a baby by emergency C-section if necessary.
GIVING BIRTH AT HOME INCREASES BABY’S RISK OF EXPERIENCING A BIRTH INJURY
A recent Oxford University study found that babies born at home to first-time mothers are almost 3 times more likely to suffer a major complication or die. Giving birth at home is extremely risky because a prompt C-section delivery cannot occur if the baby experiences a complication. If a baby is not quickly delivered when she experiencing a lack of oxygen to her brain, she can suffer permanent brain damage such as cerebral palsy.
In a hospital, it is the standard of care to closely monitor the baby’s heart rate during labor and delivery. If the baby starts to experience birth asphyxia, this will be reflected in the fetal heart tracings on the heart monitor. When the heart tracings are non-reassuring, the physician can quickly deliver the baby by an emergency C-section in order to prevent brain damage. In a home setting, if the baby starts to experience birth asphyxia, valuable time is wasted transporting the mother and baby to a hospital where a C-section can be performed and the baby can receive critical medical intervention. It is imperative that emergency interventions, such as delivery and resuscitation, not be delayed.
Most babies are born with no serious complications. But in the event that a complication does occur, it is crucial that the situation be medically managed right away to prevent the baby from having permanent disabilities such as cerebral palsy. Medical experts say that labor and delivery is a time of high risk and that home births expose babies to an unreasonable risk of potentially lifelong disabilities.
Of course, there are benefits to delivering a baby at home. But mothers can obtain many of these benefits in labor and delivery units that mimic a home setting. In these units, women can have water births and relaxing therapies such as hypnobirthing and foot massages. The benefit of having a “home birth” at a medical facility is that there is a medical team that can closely monitor the baby’s heart rate and quickly deliver the baby by C-section if needed.
If a mother is giving birth at a medical facility that holds itself out as a labor and delivery unit, the baby’s heart rate must be closely monitored and skillfully interpreted at the start of admission. If the baby’s heart rate becomes non-reassuring or there is a complication occurring indicative of impending fetal distress, the baby must be quickly delivered, usually by C-section. Failure to monitor and properly interpret the baby’s heart rate, and failure to quickly deliver the baby when necessary are negligence. If this negligence causes the baby to have permanent brain damage and lifelong conditions such as cerebral palsy, a seizure disorder, intellectual disabilities, developmental delays, hydrocephalus or periventricular leukomalacia (PVL – mostly seen in premature infants), it is medical malpractice.
AWARD WINNING BIRTH BRAIN INJURY LAWYERS HELPING CHILDREN FOR ALMOST 3 DECADES
 If you are seeking the help of a lawyer, it is very important to choose a lawyer and firm that focus solely on birth injury cases. Reiter & Walsh ABC Law Centers: Birth Injury Lawyers is a national birth injury law firm that has been helping children with birth injuries for almost 3 decades.
If you are seeking the help of a lawyer, it is very important to choose a lawyer and firm that focus solely on birth injury cases. Reiter & Walsh ABC Law Centers: Birth Injury Lawyers is a national birth injury law firm that has been helping children with birth injuries for almost 3 decades.
Birth injury lawyer Jesse Reiter, president of ABC Law Centers: Birth Injury Lawyers, has been focusing solely on birth injury cases for over 28 years, and most of his cases involve hypoxic ischemic encephalopathy (HIE) and cerebral palsy. Partners Jesse Reiter and Rebecca Walsh are currently recognized as two of the best medical malpractice lawyers in America by U.S. News and World Report 2015, which also recognized ABC Law Centers: Birth Injury Lawyers as being one of the best medical malpractice law firms in the nation. The lawyers at ABC Law Centers: Birth Injury Lawyers have won numerous awards for their advocacy of children and are members of the Birth Trauma Litigation Group (BTLG) and the Michigan Association for Justice (MAJ).
If your child was diagnosed with a birth injury, such as cerebral palsy, a seizure disorder or hypoxic ischemic encephalopathy (HIE), the award-winning birth injury lawyers at ABC Law Centers can help. We have helped children throughout the country obtain compensation for lifelong treatment, therapy and a secure future, and we give personal attention to each child and family we represent. Our nationally recognized birth injury firm has numerous multi-million dollar verdicts and settlements that attest to our success and no fees are ever paid to our firm until we win your case. Email or call Reiter & Walsh ABC Law Centers: Birth Injury Lawyers at 888-419-2229 for a free case evaluation. Our firm’s award-winning birth injury lawyers are available 24 / 7 to speak with you.