Uterine Rupture and Birth Injury
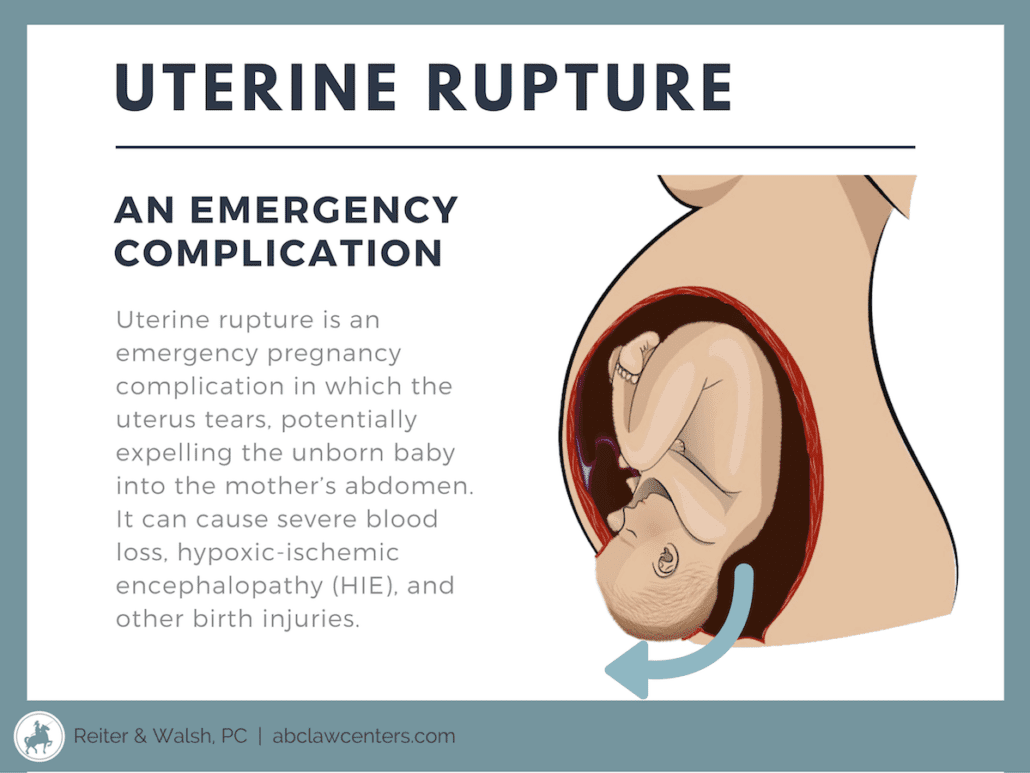
A uterine rupture is a tear in the uterus during pregnancy, labor, or delivery. It is an obstetrical emergency that requires immediate delivery. The uterus can rupture throughout some or all of its layers, reducing the baby’s oxygen supply and causing severe bleeding for the mother. A ruptured uterus often causes the baby to move into the mother’s abdomen before delivery.
A uterus rupture is most common among women undergoing TOLAC (trial of labor after cesarean) or VBAC (vaginal birth after cesarean) deliveries. It usually occurs because the scars from previous C-sections or uterine or abdominal surgeries tear during labor.
Did you have a uterine rupture during labor?
You’re not alone, and you have options. Speak to one of our birth injury lawyers to learn more.
What Are The Complications Of A Uterine Rupture?
The uterus, or womb, holds the baby and the amniotic fluid inside. The placenta is attached to the inside of the womb, and the umbilical cord is attached to the placenta. Oxygen-rich blood flows from the blood vessels in the womb to the placenta and goes through the umbilical cord vein to the baby. Certain blood vessels of the uterus and placenta are part of what’s called uteroplacental circulation, which brings the blood to the umbilical cord.
If the uterus ruptures, the baby can become severely deprived of oxygen (birth asphyxia) and develop a brain injury called hypoxic-ischemic encephalopathy (HIE), which can cause seizures, cerebral palsy, developmental delays, and more. If a uterine rupture occurs when the baby is premature, birth asphyxia may cause brain injuries that can lead to death or permanent damage. Premature babies are also at higher risk of experiencing apnea and bradycardia because their organs are not yet fully developed before birth.
The complications of a uterine rupture depend on the duration of time between its diagnosis and the baby’s delivery. It is critical that medical professionals monitor the mother’s labor, quickly diagnose a uterine rupture, and deliver immediately. According to a study in the American Journal of Obstetrics and Gynecology (AJOG), significant newborn injury was found in cases of uterine rupture when the baby was delivered more than 18 minutes after the uterus ruptured. As such, there is a low threshold for suspicion of uterine rupture and emergency C-section during a trial of labor after C-section (TOLAC).
Sadly, a ruptured uterus can lead to fetal complications such as birth asphyxia and neonatal death. When a uterine rupture occurs, roughly six percent of babies die. If you experienced any of these situations after a uterine rupture, consider speaking with a dedicated birth injury attorney to better understand your legal options.
What is Birth Asphyxia?
Birth asphyxia occurs when a baby does not get enough oxygen in the womb prior to delivery and is usually caused by a uterine tear. The location and extent of the uterine tear and the baby’s health status play a role in how severe the birth asphyxia will be.
Regardless of the extent of the uterus rupture, medical professionals must immediately intervene in order to prevent a lack of oxygen to the baby’s brain. The baby must be delivered by emergency C-section as soon as a uterine rupture occurs, or the situation could qualify as medical malpractice.
A ruptured uterus can cause the baby to experience birth asphyxia in several situations, such as the following:
- The tear causes the mother to lose so much blood that it diminishes or cuts off the baby’s blood and oxygen supply. A severe hemorrhage could send the mother into shock, which is life-threatening for her and the baby.
- The rupture is at or very close to the placenta, and it severs blood vessels that send oxygen-rich blood to the baby.
- The rupture could dislodge the placenta. Placental abruption and uterine rupture can occur together.
- If the baby starts to move into the mother’s abdomen when the uterus is ruptured, many serious medical complications can occur. For example, the umbilical cord can stretch, compress, or tear.
Possible Maternal Complications From a Ruptured Uterus
A ruptured uterus can lead to maternal complications such as severe blood loss or hemorrhage, the need for a hysterectomy, and maternal death. Thankfully, less than 1% of mothers who experience a ruptured uterus die from this condition.
What Are the Risk Factors For a Uterine Rupture?
Uterine Scars
- Uterus scars that can increase the risk of uterine rupture include:
- Scar from a C-section
- High vertical or fundal hysterotomy scar
- Uterine perforation scar: This can occur as a result of any complication involving the uterus and transcervical procedures
- Myomectomy or metroplasty scar: These scars are from the removal of fibroids in the uterus
- Scar from the previous repair of a ruptured uterus
During pregnancy, scars should be imaged. When a doctor finds a thin scar or defect, they should be concerned about a possible uterine rupture during labor as well as during pregnancy and take steps to address potential problems.
The rupture of an unscarred uterus is rare, only happening once in every 5,700 to 50,000 pregnancies. In one case study, Only 13% of all uterine ruptures occurred for women with an unscarred uterus.
An unscarred uterus may rupture from:
- trauma (as in an accident or a fall)
- weakness in the middle layer of the uterine wall (which induces contractions)
- abnormal architecture of the uterine cavity.
Vaginal Birth After C-Section (VBAC)
VBAC (vaginal birth after c-section) delivery puts patients at risk for uterine rupture because of the pressure placed on the scar tissue in the uterus. Additionally, administering labor drugs such as Pitocin to induce labor in a patient who had a previous C-section can increase this risk.
Most uterine ruptures occur because the uterus is scarred from a previous C-section. Some are classical C-section scars, which are longitudinal (across the abdomen) upper-segment scars. These scars can not only rupture during labor and delivery, but also during pregnancy. Rupture of lower segment C-section scars usually takes place during labor.
Physical Risk Factors
Overdistention of the uterine cavity, which can occur when the mother is carrying a large baby or multiple babies, is the major physical factor in uterine rupture cases. Also, labor that takes longer than expected due to slow cervical dilation can place prolonged stress on the uterine wall, leading to the loss of the wall’s integrity.
Risk factors for uterine rupture involving overdistention and prolonged physical stress include:
- Abnormal fetal position or presentation
- Post-term labor: Labor past 40 weeks
- Recent delivery (within less than 18-24 months)
- One or more previous cesarean deliveries
- Single-layer uterine closure in prior C-section
- Macrosomia or a baby that is large for gestational age (LGA) (over 8 lbs)
- Multiple fetuses (twins, triplets, etc.)
- Labor dystocia (difficult labor), particularly at advanced gestation
- Certain obstetric maneuvers, such as internal version (physician’s adjustment of the baby’s position in the womb by placing one hand in the mother’s vagina and the other on her abdomen)
Preventing uterine rupture

The best way to prevent uterine rupture is to perform a planned cesarean birth. In the case of a TOLAC, it is necessary to carefully determine which patients are at risk for uterine rupture before it occurs. Physicians must be aware of the mother’s medical history and closely watch her during pregnancy and labor.
Great effort must be made in diagnosing even minor degrees of CPD (Cephalopelvic disproportion) where the mother’s pelvis is too small for the size of the baby’s head or malpresentation and other risk factors, especially placental abruption. Mothers with risk factors should be attended to and treated in a special high-risk intensive care zone in the labor department by specially trained physicians and personnel. Difficult deliveries should not be attempted; instead, C-section delivery should be planned and performed.
A vaginal birth after C-section (VBAC) should be attempted only by skilled and prepared professionals who are immediately available for emergency delivery and only with the mother’s informed consent.
If any of these precautions or procedures were not taken during your child’s birth and you experienced a ruptured uterus and your child suffered HIE or another birth injury, you may have the right to request compensation for the emotional and financial losses you suffered. The dedicated birth injury lawyers at ABC Law Centers can answer all your questions and explain your legal rights during a free consultation. Contact us to learn more today.
What Are the Symptoms and Signs of Uterine Rupture?
It is critical for the medical team to closely monitor a mother and baby during labor and delivery – and throughout pregnancy – so that dangerous conditions such as a ruptured uterus can be promptly treated.
Some of the symptoms and signs of uterine rupture include the following:
- Abnormal fetal heart rate (FHR): non-reassuring heart tracings, fetal heart rate decelerations.
- Vaginal bleeding or hemorrhaging
- Sudden abdominal pain
- Changes in contraction patterns
- Baby recedes back into the birth canal (loss of station)
- Hemodynamic instability (blood pressure and heart rate problems)
- Hematuria if the rupture extends into the mother’s bladder
Non-reassuring fetal heart tones, bleeding, or pain are the most common signs of uterine rupture, and only one of these situations is needed to suspect rupture. In some cases, signs of fetal distress will appear before pain or bleeding. The fetal heart rate monitor shows physicians how the baby is tolerating labor. It is critical that physicians pay close attention to the fetal heart monitor and be prepared to perform an emergency C-section if the baby shows signs of distress.
When a ruptured uterus occurs, a prompt delivery by emergency C-section must follow. Severe abdominal pain, fetal heart rate abnormalities, and unstable blood flow to the baby usually require an emergency C-section, regardless of the cause.
How Medical Staff Should Manage Uterine Rupture
Medical teams are obligated to take several steps to address uterine rupture symptoms and manage a uterus rupture. If they fail to use proper medical care or negligently perform procedures that result in a birth injury, each state provides legal remedies to help protect the mother and child in these serious circumstances.
To learn how your state’s laws protect you and your child, reach out to the birth injury team at ABC Law Centers today.
Here are some of the acts a responsible labor and delivery team should consider when faced with the signs of a uterine rupture:
BEFORE LABOR
Uterine rupture may be suspected before delivery because of one or more of the signs and symptoms mentioned above. If this is the case, a a C-section will usually be performed, even if a uterine rupture is not diagnosed.
DURING LABOR
If a uterine rupture occurs during labor, doctors will need to perform an emergency C-section immediately. The goals of the surgery are to deliver the baby safely, control hemorrhage in the mother, repair the uterus, identify damage to other organs, and minimize post-surgical complications or death. In some cases, however, the doctor must perform a hysterectomy, which is the complete removal of the uterus.
DELIVERY
A fast delivery is imperative in cases of uterine rupture in order to avoid harm to both mother and baby. The delivery should occur within 18 minutes of uterine rupture in order to avoid brain injury to the baby from not getting enough oxygen.
What Are the Long-Term Outcomes of a Mismanaged Uterine Rupture?
When uterine rupture causes birth asphyxia, this may lead to permanent brain injury and a variety of disabilities, such as:
- Neurological impairment
- hypoxic-ischemic encephalopathy (HIE)
- cerebral palsy
- developmental delays
If you and your child are facing any of these medical concerns after a mismanaged uterine rupture or other form of medical malpractice during the birth process, you don’t have to face the future alone. Our compassionate birth injury attorneys are ready to guide you through the legal process.
We can help you recover the financial compensation you and your child need for the medical care and accommodations you both deserve, now and in the future. Contact our dedicated team today.


Trusted Birth Injury Lawyers: Handling Uterine Rupture Cases Since 1997
Birth injury cases require specific, extensive knowledge of both law and medicine. To achieve the best results for our clients, our team at ABC Law Centers exclusively handles birth injury cases. Our team has the qualifications, experience, and accomplishments that contribute to our consistent success.
We’ve successfully handled cases involving dozens of different complications, injuries, and instances of medical malpractice related to obstetrics and neonatal care. Our clients hail from all over the United States, and we partner with a network of birth injury attorneys in every state to help families like yours nationwide.
Contact our birth injury attorneys and intake nurse with any questions you may have. We do not charge legal fees for our services unless we successfully resolve your case and recover compensation for you!
Featured Videos
Posterior Position
Hypoxic-Ischemic Encephalopathy (HIE)

Featured Testimonial
What Our
Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on. ABC Law Centers: Birth Injury Lawyers was just that.
- Michael
Helpful resources
- Uterine rupture: After previous cesarean birth – UpToDate
- A Case Series of Uterine Rupture: Lessons to be Learned for Future Clinical Practice – PubMed
- Uterine Rupture: Causes, Symptoms, and Treatment – Healthline
- Uterine rupture after previous cesarean delivery: Maternal and fetal consequences – PubMed
- Uterine rupture: Unscarred uterus – UpToDate
- Uterine Rupture: What Family Physicians Need to Know | AAFP
- Uterine Rupture: Signs, Symptoms, Risks & Treatment – Cleveland Clinic


